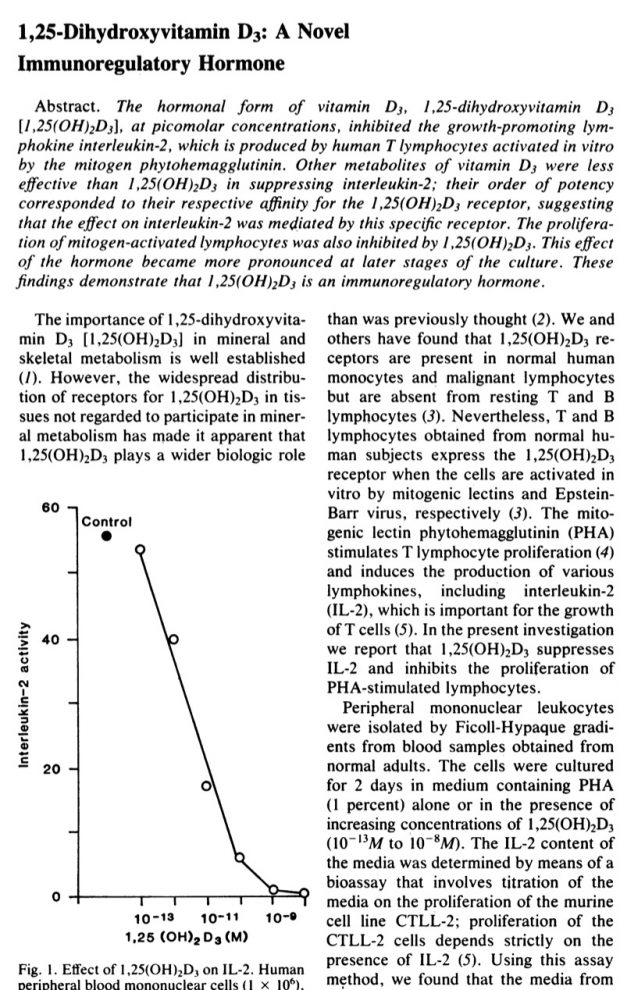
Vitamin D was introduced into clinical medicine in 2 large waves basically in the 1930ies and 1960ies without any clinical study.
Although I am interested in the relationship twith allergy since 1999 none of our proposed four vitamin D trials were funded.
2005: “Vitamin D and Induction of Allergies”
2013: “Vitamin D and allergy (VIT-AL)”
2017: “Biomarker Screening of Vitamin D response in Newborns (VITAPRIME)”
2017: “Immunological effects of vitamin D supplementation in newborns in Ghana (IMVITAD-GHA)”
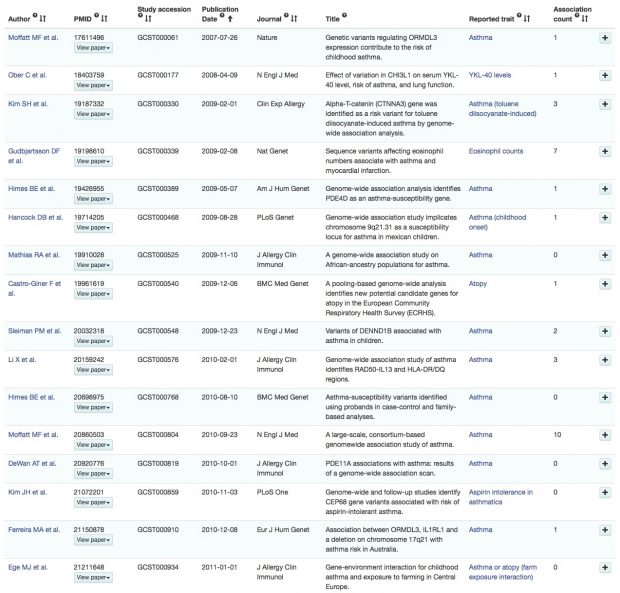
Unfortunately the published clinical studies so far missed the point as they were looking only at pregnancy and not at newborn supplements (VDAART, COPSAC and Grant/NZ).
But there are good news now, as studies are going on in Australia and Finland that are sufficiently powered and examining exposure in the newborn period: VIDI and VITALITY. The only problem there will be the inevitable co-exposure by vitamin D supplemented baby food.