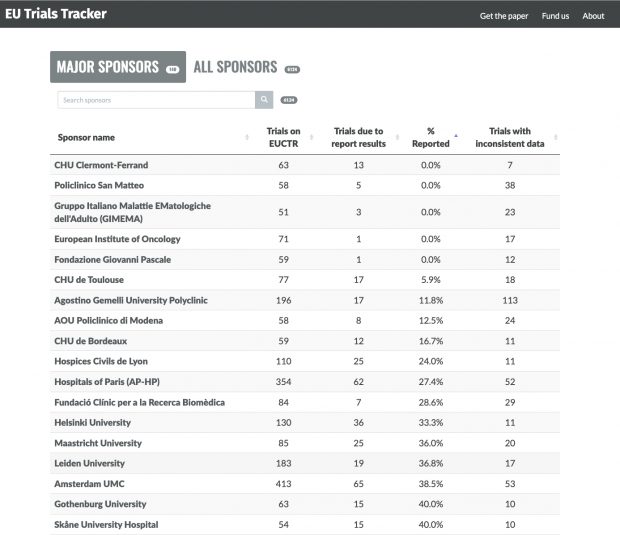
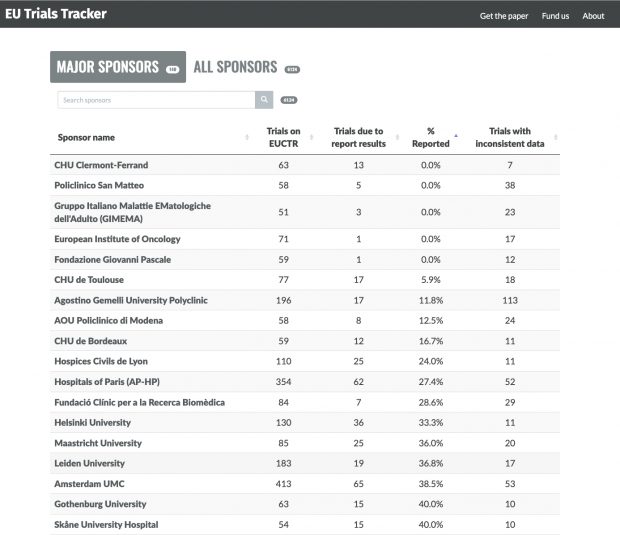
The British trials tracker, a never ending list of fame and shame
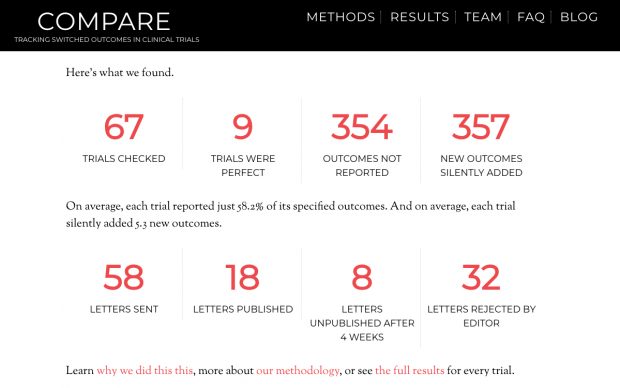
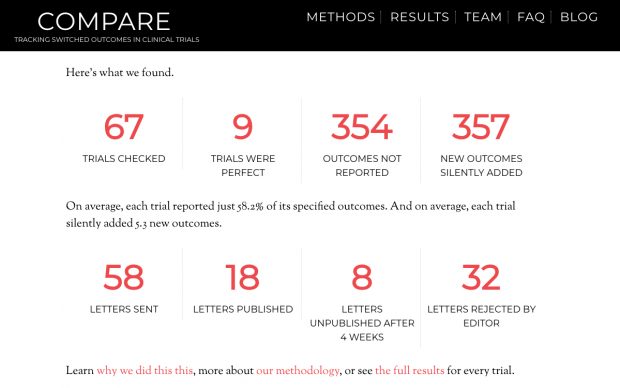
Although limited in scope, the COMPARE website of switched outcomes is also entertaining.
The British trials tracker, a never ending list of fame and shame
Although limited in scope, the COMPARE website of switched outcomes is also entertaining.
“Free synthetic data”? There are numerous Google ads selling synthetic aka fake data. How “good” are these datasets? Will they ever been used for scientific publications outside the AI field eg surgisphere-like?
There is a nice paper by Taloni, Scorcia and Giannaccare that tackles the first question. Unfortunately a nature news commentary by Miryam Naddaf is largely misleading when writing Continue reading Can ChatGPT generate a RCT dataset that isn’t recognized by forensic experts?
A new study by Urashima et al. shows that sensitization to cow’s milk and food allergy, including CMA and anaphylaxis, is preventable by avoiding CMF (cow milk formula) supplementation for at least the first few days of life. Although examined only indirectly in this study, vitamin D supplementation seems to be involved in the sensitization process.
Note to self – here is a list of all vitamin D / allergy related clinical trials following the first case report was Moneret-Vautrin DA, Hatahet R, Kanny G, Ait-Djafer Z. Allergenic peanut oil in milk formulas. The Lancet 1991; 338: 1149. doi: 10.1016/0140-6736(91)92008-p.
1. De Montis G, Gendrel D, Chemillier-Truong M, Dupont C. Sensitisation to peanut and vitamin D oily preparations. The Lancet 1993; 341: 1411. doi: 10.1016/0140-6736(93)90976-N.
2. De Montis G, Gendrel D, Chemillier-Truong M, Dupont C. [Peanut sensitization and oily solution vitamin preparations]. Arch Pediatr 1995;2(1):25-8. doi: 10.1016/0929-693x(96)89804-6.
3. Rueter K, Jones AP, Siafarikas A, Lim EM, Bear N, Noakes PS, et al. Direct infant UV light exposure is associated with eczema and immune development. J Allergy Clin Immunol 2018; in press, doi: 10.1016/j.jaci.2018.08.037.
4. Rosendahl J, Pelkonen AS, Helve O, et al. High-Dose Vitamin D Supplementation Does Not Prevent Allergic Sensitization of Infants. J Pediatr. 2019 Jun;209:139-145.e1. doi: 10.1016/j.jpeds.2019.02.021
The Urashima study is accompanied by a valuable editorial of George du Toit and Kari Nadeau
There is currently a lack of consensus among national allergy societies .. Although the EAACI3 and American Academy of Allergy, Asthma and Immunology (AAAI) currently recommend the use of hypoallergenic formulas in infants at high risk of allergy, the Australian Society of Clinical Immunology and Allergy does not. The EAACI and the AAAI are likely to reconsider their guidelines because results of more re- cent studies have been contradictory. … Guidelines in the United States and United Kingdom recommend routine vitamin D supplementation in all breastfed infants, whereas guidelines in Australia recommend supplementation only in breastfed infants at high risk of vitamin D insufficiency.
Nearly forgot to mention the new study of Jenni Rosendahl who compared high-dose to low-dose vitamin D supplementation effects. The Vitamin D Intervention in Infants (VIDI) study was a randomized controlled 24-month trial of daily 400 IU or 1200IU vitamin D supplementation administered to healthy infants that evaluated the effect of vitamin D supplementation on bone health and infections.
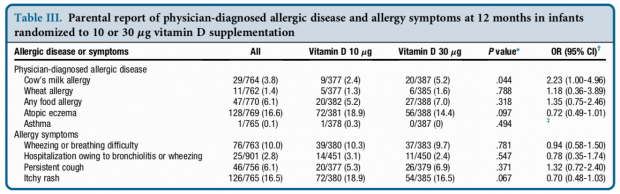
I would say sensitization against one of the most common allergen in this age group happens already in the low dose group while the higher dose leads to a further 2.2fold increased disease risk.
Would be really important to have any unexposed control group here.
Are there any news in the allergy & vitamin D controversy?
Unfortunately there are still no results from VDAART study on early vitamin D effects – even after so many years (and expenses of >10M $). Continue reading Ceterum censeo I
After more than a century of research, the first successful clinical trial of an allergy risk factor has been performed. It looks like the authors even did not anticipate such an effect (known as triple blind design). But read what the Pubmed article about the Norizoe et al. paper says
To elucidate whether maternal vitamin D supplementation during lactation improves infantile eczema and other subsequent allergic disorders, a randomized, double-blind, placebo-controlled trial was performed.
Mothers (n=164) of infants with facial eczema at one-month checkup were randomly assigned to receive vitamin D3 supplements (n=82; 800 IU/day) or placebo (n=82) for 6 weeks from May 2009 to January 2011. The primary outcome was infantile eczema quantified by Scoring Atopic Dermatitis (SCORAD) index at the three-month checkup, and the secondary outcomes were atopic dermatitis, food allergy, and wheeze diagnosed by doctors up to 2 years of age.
There was no significant difference in SCORAD at 3-month checkup between two comparative groups. Doctor-diagnosed food allergy was significantly more common up to age 2 years in vitamin D group (10/39: 25.7%) than in placebo group (3/40: 7.5%; RR=3.42, 95%CI=1.02 to 11.77, P=0.030). Moreover, at least one secondary outcome was also significantly more common in vitamin D group (17/39: 43.6%) than in placebo group (7/40: 17.5%; RR=2.49, 95%CI=1.16 to 5.34, P=0.012).
These results suggest that vitamin D supplementation may not decrease the severity of infantile eczema at three months of age, but may rather increase the risk of later food allergy up to two years of age. Because a large number of subjects was lost to follow-up, further study is needed to confirm the findings.
Of course, there may be some weakness in the study design, a large loss to follow-up and the way how food allergy was diagnosed will be critized. I think, however, that this is a major breakthrough that raises the hope that we will finally understand how allergy develops.
I should have added “true” risk factor, as there are positive trials on probiotics and atopic dermatitis. The meta-analysis by Lee immediately lead to a rebuttal
Their review fails to meet published standards for the quality of systematic reviews on several criteria, and this has led to inappropriate conclusions. […] These defects in methodologic rigor have led to an exaggeration of the clinical benefits of probiotics for eczema prevention.
The Cochrane Summaries are also negativ
There is not enough evidence to recommend using probiotics for the treatment of eczema.
Same situation with asthma
We found no evidence to support a protective association between perinatal use of probiotics and doctor diagnosed asthma or childhood wheeze
The title says it all – the link goes to to the add-ons page, a very handy template Continue reading Consort study diagrams available with Omnigraffle