A randomized controlled study of pregnant women examined 400 IU vitamin D3 vs 3,800 IU from the second trimester through 4-6 weeks postpartum by genome-wide DNA methylation in leukocytes.
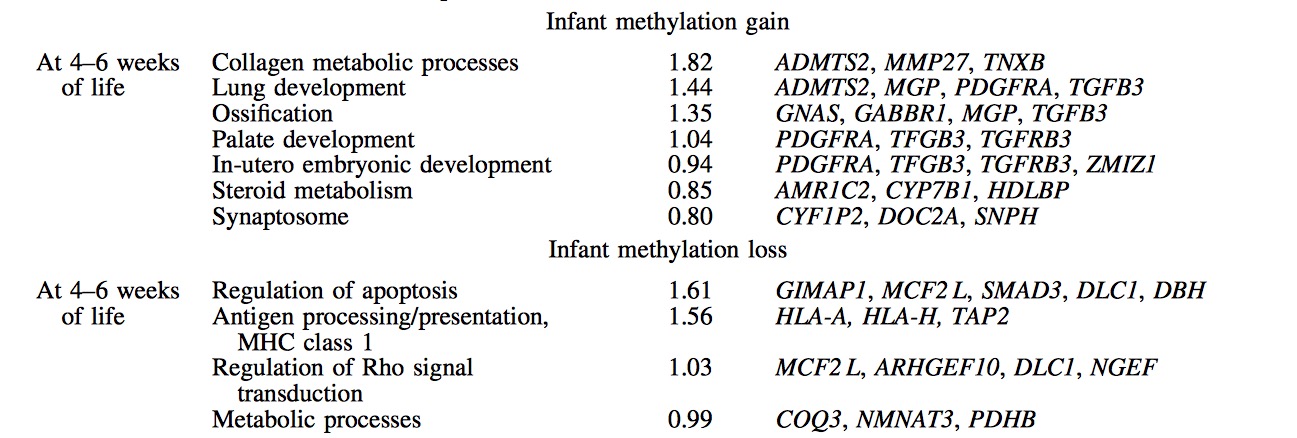
At birth, intervention group mothers showed DNA methylation gain and loss at 76 and 89 cytosine- guanine (CpG) dinucleotides, respectively, compared to controls. Postpartum, methylation gain was noted at 200 and loss at 102 CpGs. Associated gene clusters showed strongest biologic relevance for cell migration/ motility and cellular membrane function at birth and cadherin signaling and immune function at postpartum.
It seems that D3 supplementation is generating epigenetic effects in the offspring, something that we predicted already in 2012 as programming of vitamin D sensitivity.
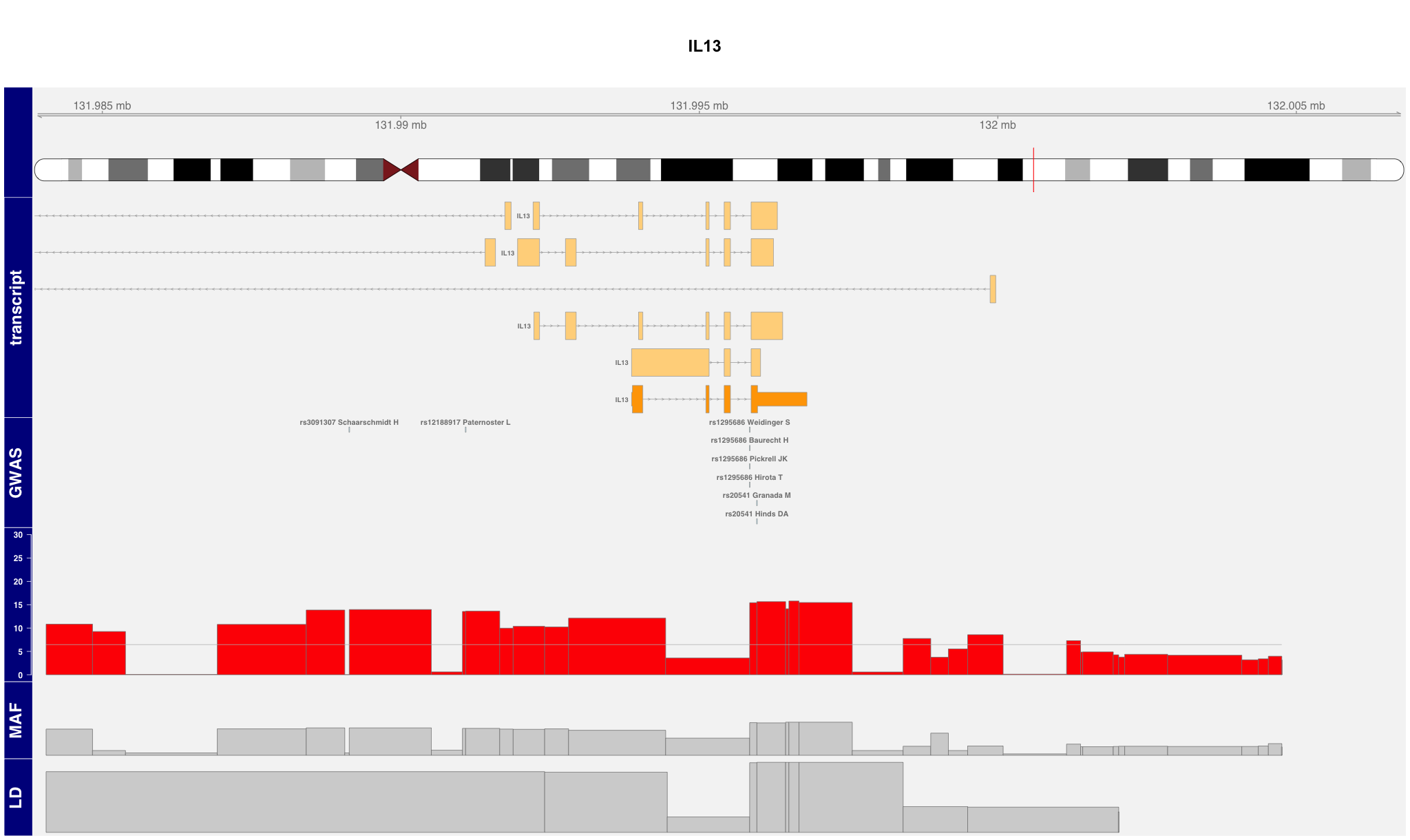
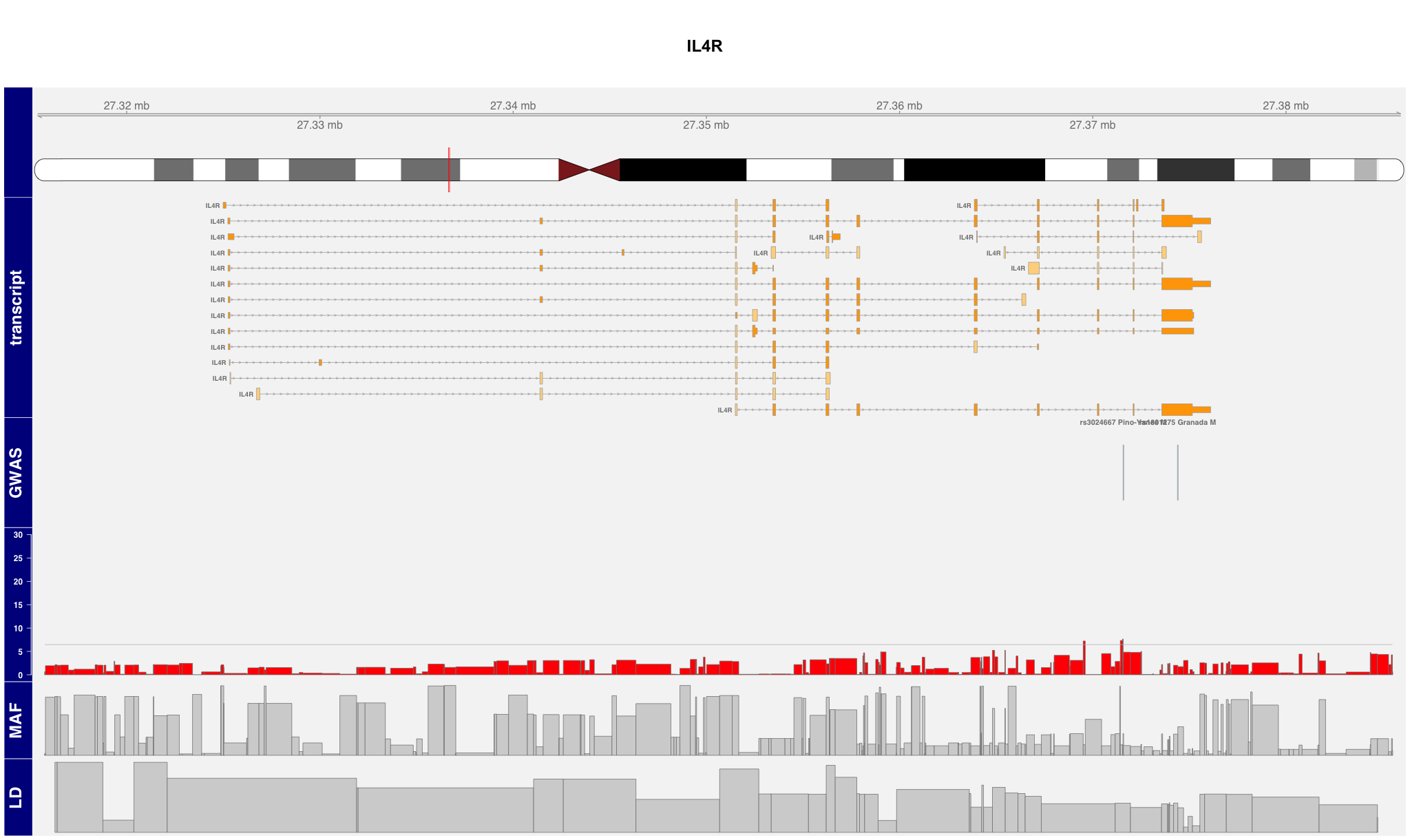
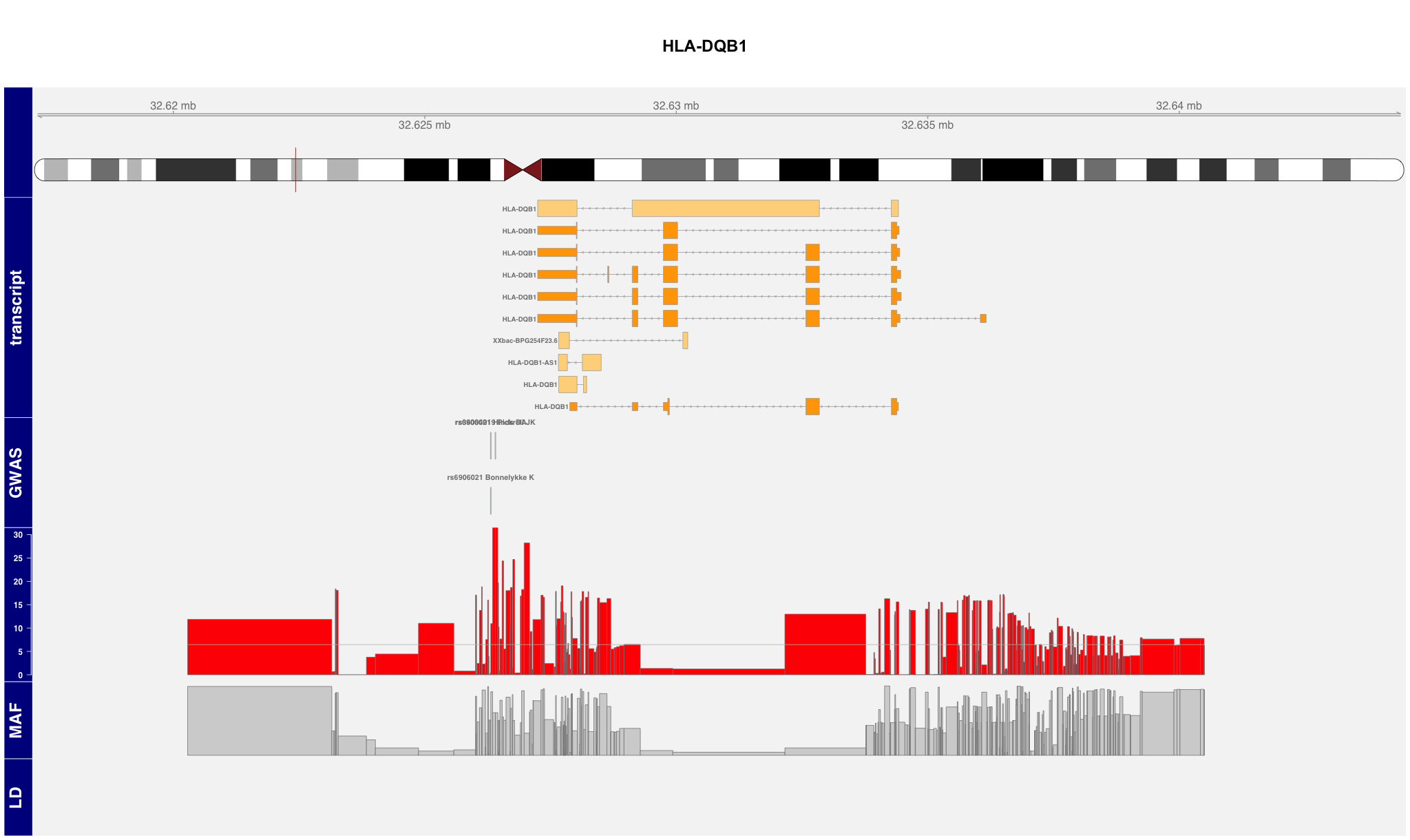
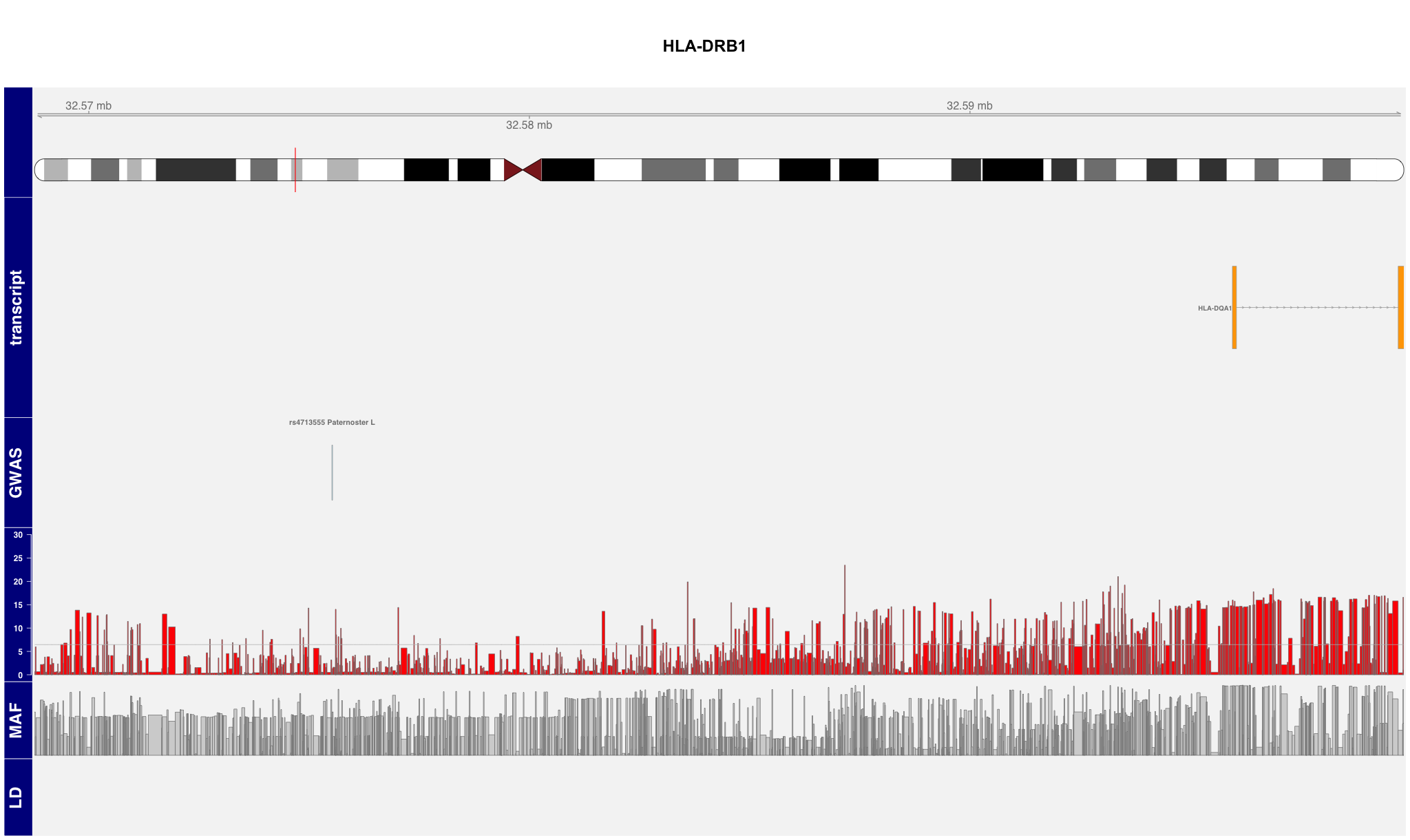
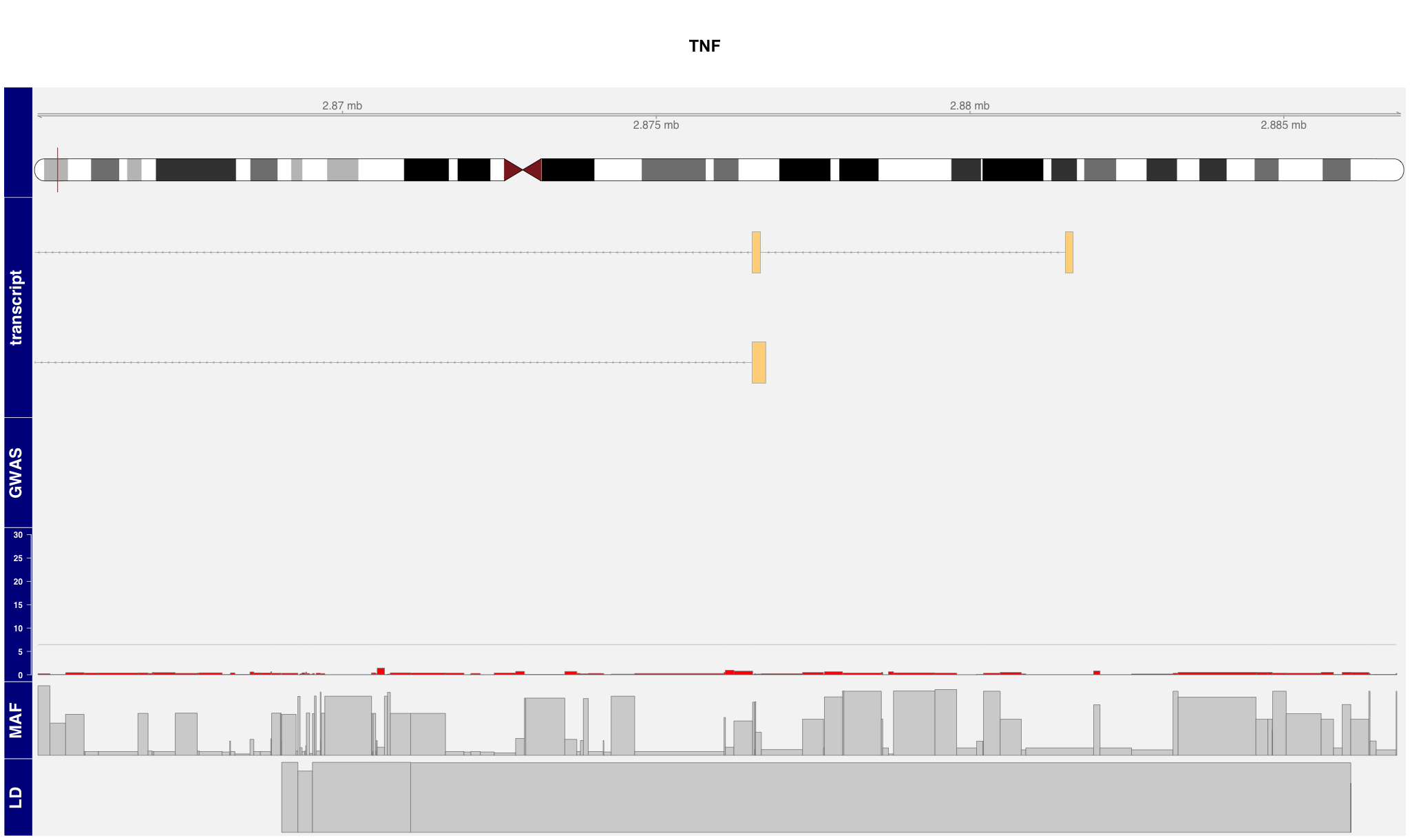
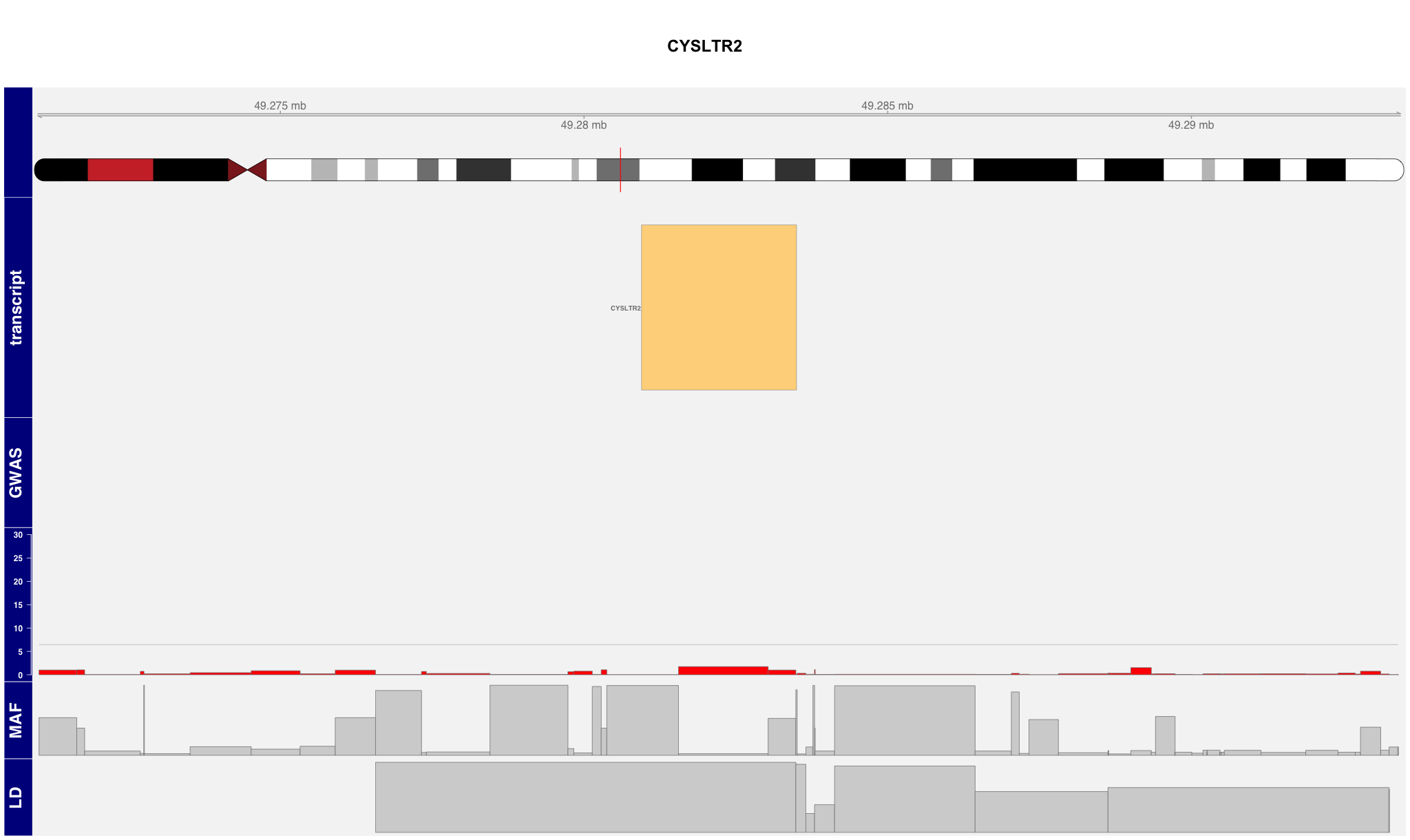
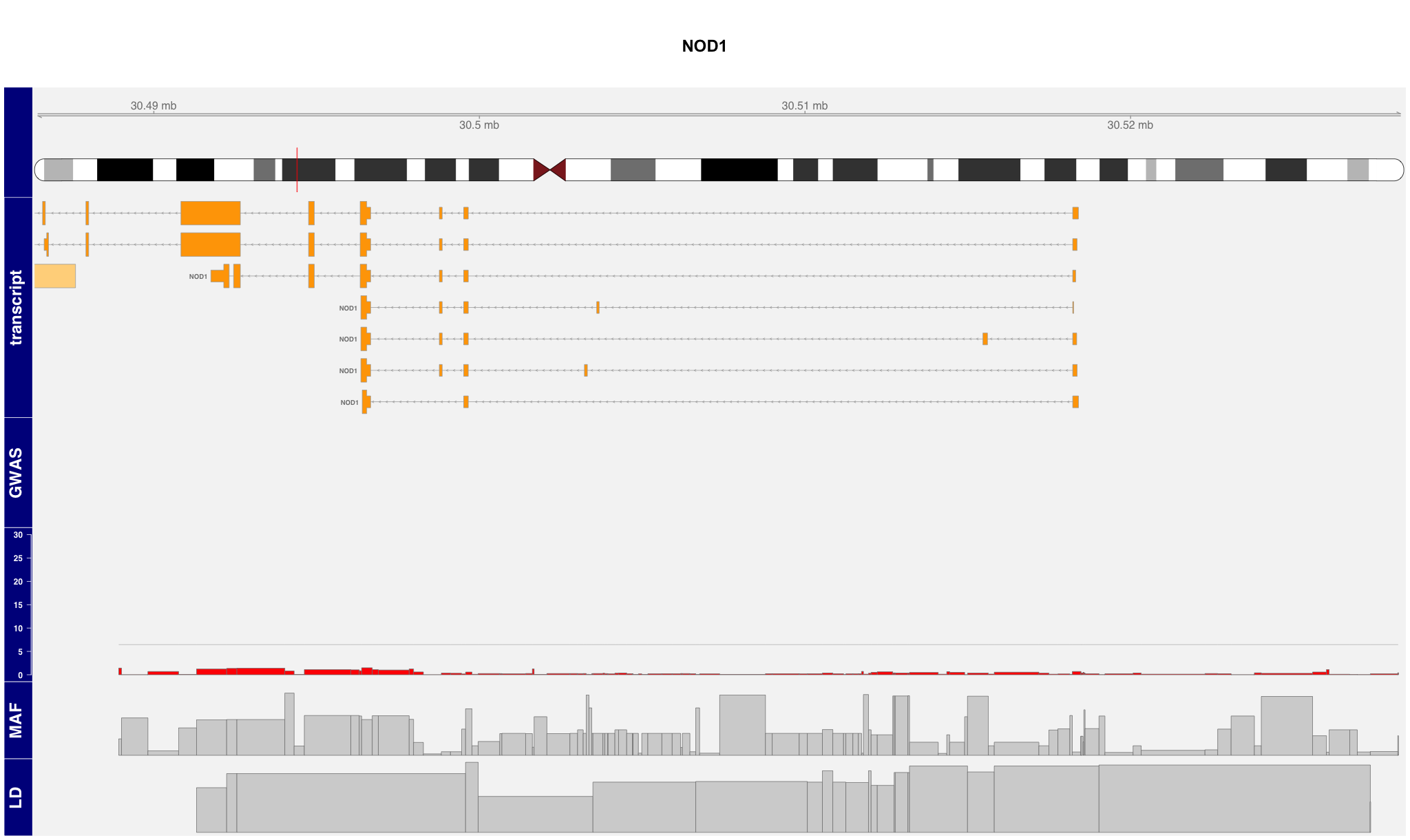
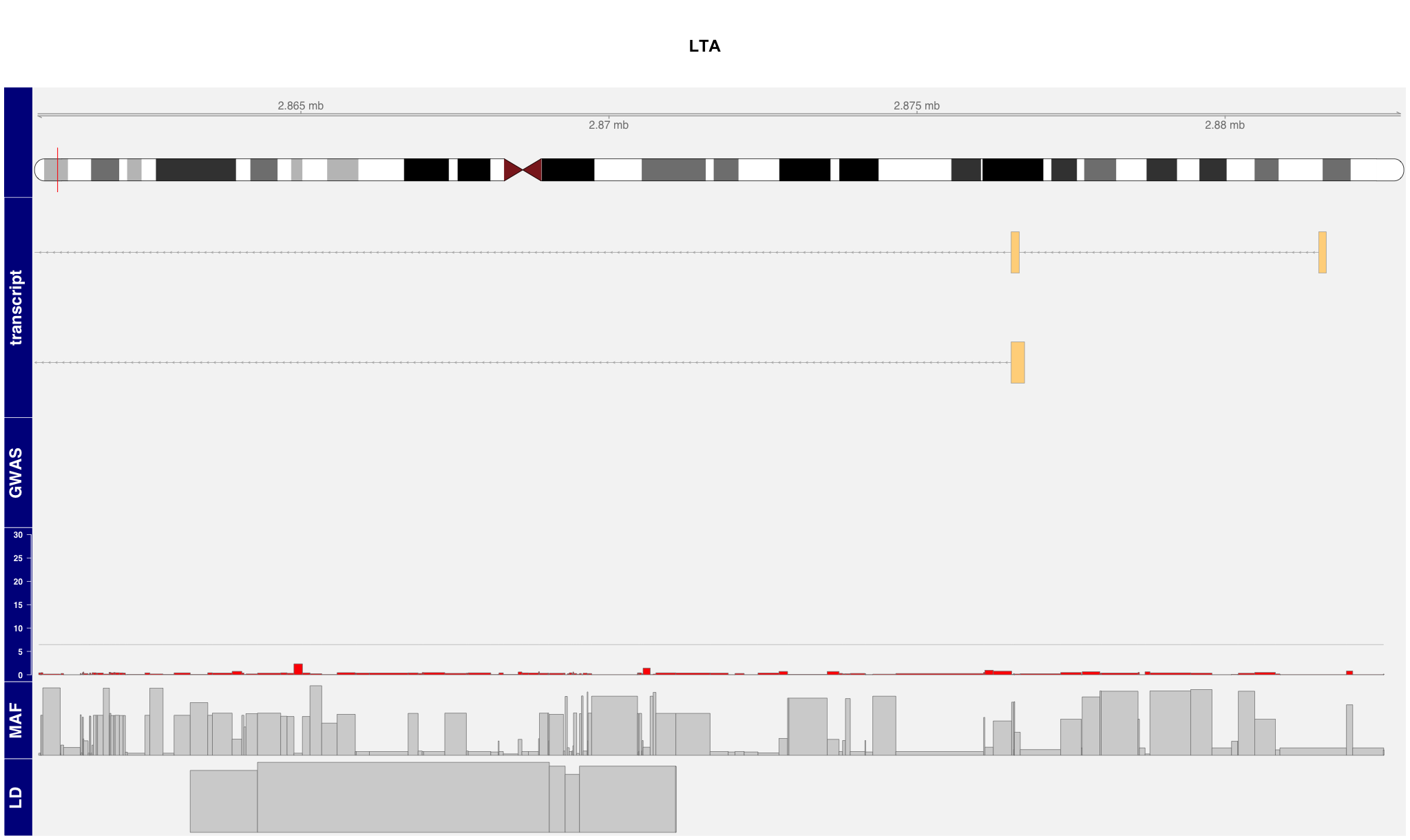
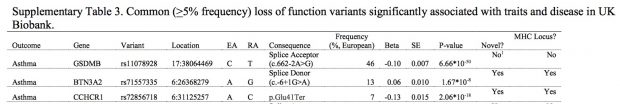
When re-annotating the genes above using biocLite(“mygene”) there are at least 2 interesting genes for gain of methylation are getting to the surface: ZMIZ1 T cell differentiation) and CYP7B1 (first reaction in the cholesterol catabolic pathway of extrahepatic tissues, which converts cholesterol to bile acids). But also methylation loss is interesting with HLA-A (antigen processing).