Last Word on Nothing writing about ChatGPT
What initiated my change of mind was playing around with some AI tools. After trying out chatGPT and Google’s AI tool, I’ve now come to the conclusion that these things are dangerous. We are living in a time when we’re bombarded with an abundance of misinformation and disinformation, and it looks like AI is about to make the problem exponentially worse by polluting our information environment with garbage. It will become increasingly difficult to determine what is true.
Is “derivate work” now equal to reality? Here is Geoff Hinton
“Godfather of AI” Geoff Hinton, in recent public talks, explains that one of the greatest risks is not that chatbots will become super-intelligent, but that they will generate text that is super-persuasive without being intelligent, in the manner of Donald Trump or Boris Johnson. In a world where evidence and logic are not respected in public debate, Hinton imagines that systems operating without evidence or logic could become our overlords by becoming superhumanly persuasive, imitating and supplanting the worst kinds of political leader.
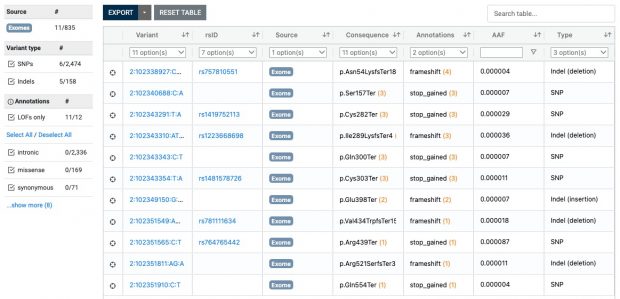
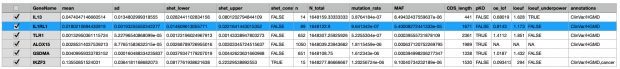
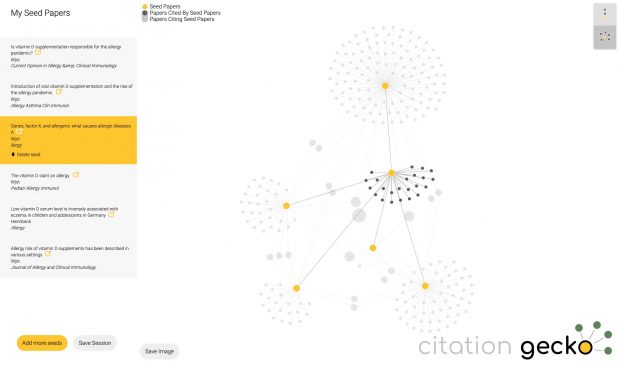
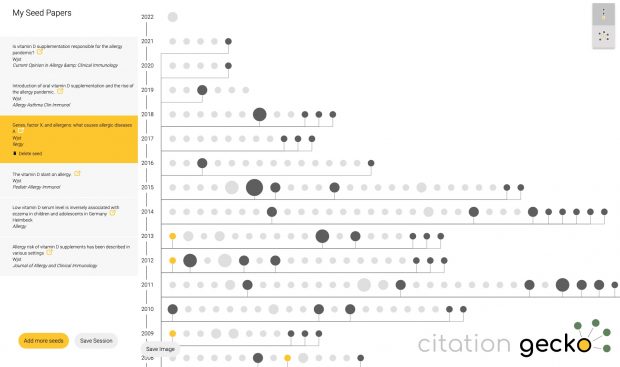
At least in medicine there is an initiative underway where the lead author can be contacted at the address below.
In my field, the first AI consultation results look more than dangerous with one harmful response out of 20 questions.
A total of 20 questions covering various aspects of allergic rhinitis were asked. Among the answers, eight received a score of 5 (no inaccuracies), five received a score of 4 (minor non-harmful inaccuracies), six received a score of 3 (potentially misinterpretable inaccuracies) and one answer had a score of 2 (minor potentially harmful inaccuracies).
Within a few years, AI-generated content will be the microplastic of our online ecosystem (@mutinyc)