A new series of pro- and con editorials in the Am J Res Crit Care Med discusses the question why in some instances mouse models have “misdirected resources and thinking”. You may have noticed that I have only rarely used animals for research; the authors of this editorial have collected empirical data on the exploding use of murine models. Despite their attractiveness from a technological point, they are often useless because
- mice do not have asthma as even the most hyperresponsive strain does not show spontaneous symptoms
- mice do not have allergy – although sensitization can be manipulated by high intraperitoneal allergen/adjuvant injection, this does not involve immediate and late airway obstruction.
- immune reaction in mice is quite different – the interfering of some substances like vitamin D cannot be reliable tested, there is no pure Th1 and Th2 reaction in human and less stronger IL-13 response
- mice typically can not be challenged with the complex (and interacting) human exposure – oxidant stress, viral infection, obesity, diet, smoke, pollutants, ….
- time course is difficult to mimicking in the mouse, there is no longterm model
- structure of mouse airways is different – there are fewer airway generations, much less hypertrophy of smooth muscle
- inflammation in mouse is parenchymal rather than restricted
- humans are outbred, mice are inbred
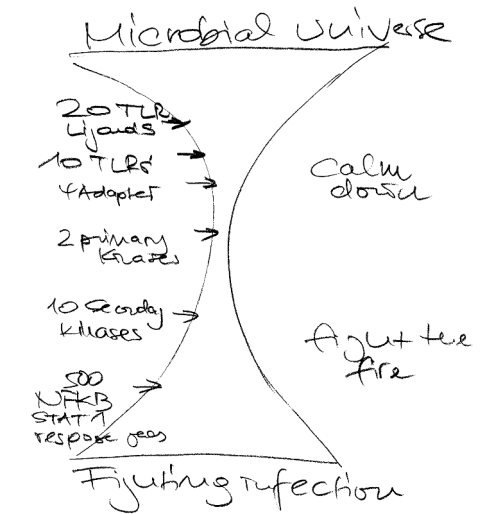
- early microbial environment is different
- many promising interventions of mice pathways failed in humans (VLA-4, IL4, IL5, bradykinine, PAF,…)
I am sure there are even more arguments – I suggest that the authors deserve the Felix-Wankel price.
Addendum
15 Dec 2006: The BMJ has 6 more examples about the discordance between animal and human studies: steroids in acute head injury, antifibrinolytics in haemorrhage, thrombolysis or tirilazad treatment in acure ischaemic stroke, antenatal steroids to prevent RDS and biphosphonate to treat osteoporosis.
19 Dec 2006: Another pitfall paper
31 Dec 2006: A blog on animal welfare
25 Apr 2007: Call for better mouse models
15 Jul 2018: Of Mice, Dirty Mice, and Men: Using Mice to Understand Human Immunology
16 Oct 2019 Allergy protection on farms – why also studies in mice could have failed
18 Feb 2023 The case for free running lab mice, see
Cell and Science paper
7 Jan 2023: A review concluding that The vitamin D system in humans and mice: Similar but not the same
12 March 2024: Limitations of the mouse model
- Lack of clinical relevance – The OVA model often fails to accurately replicate human asthma and allergic diseases. OVA is not a common human allergen, unlike house dust mites, pollen, and pet dander.
- Artificial sensitization – The model requires sensitization with alum, a strong Th2-skewing adjuvant, which does not reflect natural allergen exposure in humans.
- Simplistic immune response – OVA exposure leads to a predominantly Th2 immune response, whereas human asthma involves a complex interplay of Th1, Th2, Th17, and innate immune responses.
- Limited chronicity – Most OVA models induce short-term allergic inflammation but fail to reproduce the chronic airway remodeling, fibrosis, and structural changes seen in human asthma.
- Non-physiological exposure – OVA is often administered at high doses via intraperitoneal injection or repeated aerosol exposure, which does not mimic real-life human allergen exposure.
- Strain-specific bias – Different mouse strains respond variably to OVA, making it difficult to generalize findings.
- Lack of environmental and genetic factors – The model does not account for genetic predisposition, pollution, infections, or microbiome variations that influence human allergic disease development.
- Poor translational value – Many drugs that show promise in OVA models fail in human clinical trials, highlighting the model’s limited predictive power.
CC-BY-NC Science Surf
accessed 18.02.2026