So at week 10 after gestation, all analyzed 233 primordial germ cells lost their parental methylation marks except of 6% of the male and 8% of the female genome (which is a bit larger) . Unfortunately I did not find a list of genes there that have their parental methylation status transmitted.
Here evolutionarily young and potentially hazardous retroelements, like SVA, remain methylated ( the number of embryos being examined is not given). Evolutionarily young and potentially hazardous retroelements, like SVA, remain methylated. When testing for resistant loci, they found that H3K9me3 marked escaping ; resistant regions were also enriched for KAP1 (alias TRIM28) binding sites of ESCs. But still no gene list there.
In this paper finally there is the gene list, I was looking for — basically not demethylated, parentally inherited genes. Persistent methylated regions (also termed DMR, differential methylated regions) in advanced germline cells (AGCs) were seen in 500+ genes as given in table S4:
AADACL2-AS1, ABCA7, ABCC5, ABHD12, ABR, AC093375.1, ACSL4, ACSM1, ACVR1C, ACYP1, ADAMTSL3, ADARB2, ADK, AGBL4, AGK, AGPS, AIG1, AKAP9, AKR1B15, ALPK2, ANK1, ANKHD1, ANKHD1-EIF4EBP3, ANKRD11, ANKRD12, ANKRD19P, ANKRD20A9P, ANKRD24, ANKRD26, ANKRD26P1, ANKRD30BL, ANKRD31, AP2A2, AP3D1, AP4E1, ARAP2, ARHGAP26, ARHGAP39, ARHGAP44, ARHGEF18, ARHGEF4, ARHGEF7, ARID3A, ARL13B, ASB3, ASH1L, ASTN2, ASZ1, ATAD3A, ATF1, ATP11A, ATP13A1, ATP2C1, ATP8A2, ATP9B, AUH, AVEN, BAGE, BAGE2, BAGE3, BAGE4, BAGE5, BASP1P1, BAZ1A, BBS9, BCAS3, BCO2, BCYRN1, BEND3, BEND7, BRE, BRSK2, C14orf159, C15orf37, C1GALT1, C1orf159, C20orf196, C22orf34, C2orf61, C3orf67, C3orf67-AS1, C7orf50, C7orf60, C9orf3, CACNA1B, CACNG4, CALN1, CAMK1D, CARF, CARS2, CC2D2A, CCBL2, CCDC101, CCDC130, CCDC148, CCDC149, CCDC57, CCDC88C, CCDC97, CCNY, CCSER1, CD163, CD2AP, CD46, CDH12, CDH4, CDKAL1, CELF2, CEP70, CERK, CERS4, CFH, CHD2, CHD6, CHODL, CHRM5, CHRNA10, CHRNA4, CLEC16A, CLIC5, CLIC6, CNOT2, CNTN6, CNTNAP2, COG2, COL15A1, COL18A1, COL24A1, COL6A4P2, COLEC11, CORO2B, CPVL, CRTC3, CSMD1, CSMD2, CSNK1D, CTB-7E3.1, CTDP1, CTIF, CTNNA2, CTNNA3, CUBN, CXCR2, CXorf49, CXorf49B, CYCS, CYP3A5, DAPK2, DCDC2C, DDA1, DENND1A, DENND5A, DGUOK-AS1, DIP2C, DLG1, DLK1, DNAH6, DNAH8, DNAJC1, DNER, DOC2GP, DOCK1, DOCK7, DPP10, DSTN, DTNB, DYX1C1, DYX1C1-CCPG1, EBF3, ECHDC2, EDIL3, EEPD1, EFCAB10, EFCAB4B, EFTUD1, EHBP1, EIF2B3, ELMO1, EP400NL, EPHA6, EPPK1, ERC1, ERCC8, ERICH1-AS1, ERP44, ETFA, EVC2, EXD3, EXOC2, EYS, F11-AS1, FAAH, FAM172A, FAM174A, FAM207A, FAM209A, FAM86FP, FANCC, FBN3, FBXO39, FGD4, FGF14, FHIT, FIG4, FLJ30403, FNBP4, FOXN3, FREM3, FZR1, GABRA2, GAS6, GBP2, GCNT7, GDA, GGCX, GLCCI1, GLRA1, GLRA2, GMDS, GNAI1, GOLIM4, GPR75-ASB3, GRIK2, GRM7, GTF3C6, GTPBP10, GUSBP1, H6PD, HCCAT3, HCN4, HDAC4, HECTD4, HEG1, HPGD, HRNR, HS6ST3, HTR7, IFNAR1, IGF2BP3, IGSF11, IGSF22, IGSF9B, IL1RAPL2, IL31RA, IMMP2L, IMPG2, INF2, INTS1, INVS, IPO7, IQCF3, IQCG, IRAK1BP1, ISOC2, ISPD, ITFG1, ITGB1BP2, ITGBL1, JAM3, JAZF1, JMJD1C, KALRN, KATNBL1, KDM3B, KDM4C, KIAA0825, KIAA1328, KIF4A, KIF5B, KLHL20, KLHL3, LANCL3, LDB2, LDLRAD3, LHCGR, LINC00239, LINC00408, LINC00469, LINC00670, LINC00871, LINC00922, LINC01193, LINC01194, LINGO2, LMF1, LOC100128505, LOC100133669, LOC100188947, LOC100289333, LOC101927069, LOC101927280, LOC101927286, LOC101929064, LOC101929387, LOC102723742, LOC145837, LOC283683, LOC285768, LOC286083, LOC442132, LPA, LPPR1, LRP1B, LRRC4C, LTBP1, LUZP2, MAD1L1, MAGT1, MAML3, MAOA, MAP3K15, MAP4K5, MAPK10, MAPK8, MAPK8IP3, MAST2, MCTP1, MCU, MEF2A, MEI4, MELK, METTL15, METTL9, MFHAS1, MIR1273H, MIR518B, MIR518F, MIR520B, MIR548H2, MIR548O2, MIR6130, MIR6744, MOB3B, MOCOS, MTG1, MTMR7, MUC2, MUC5B, MUM1L1, MYO10, MYO5A, MYO9A, MYT1, MYT1L, NAA20, NAALADL2, NAT1, NAV2, NBPF10, NBPF20, NCALD, NCOA2, NEBL, NFATC3, NIFK-AS1, NIPA1, NKAIN2, NKAIN3, NLRP4, NME7, NOC4L, NONO, NPHP4, NQO2, NRXN3, NSUN6, NTSR1, NUBPL, NXN, OGG1, OR8S1, OSBP2, OSBPL6, OSMR, PACS2, PARK2, PARL, PAWR, PCBP3, PCDH19, PCDH9, PCNT, PCNXL2, PCSK6, PDAP1, PDE11A, PDE4D, PGAM1P5, PGAM5, PHKB, PHRF1, PIK3C2A, PIK3CA, PIP5K1B, PKD2L1, PKHD1, PKIB, PLCD1, PLCH1, PLEC, PLOD2, POLR1A, POMK, PPARA, PPARGC1B, PPP2R5C, PRH1, PRH1-PRR4, PRICKLE1, PRKAR1B, PRKCZ, PROSER2, PROSER2-AS1, PRR26, PRUNE2, PTCD3, PTDSS2, PTGFRN, PTPN21, PTPRD, PTPRN2, PYGB, RAB28, RAB3D, RAB3GAP2, RAB3IP, RABGAP1L, RAPGEF6, RBFOX1, RC3H2, RFX7, RGS6, RGS7, RNF115, RNH1, RNU6-52P, RNU6-81P, RPH3AL, RPIA, RPL35A, RPS6KC1, RSPH1, RYR1, S100Z, SCAPER, SCCPDH, SCEL, SCFD2, SCHLAP1, SCMH1, SDHAP3, SDK1, SEC14L1, SEC24D, SEL1L, SEMA3C, SERPINB3, SESN2, SESTD1, SETD1A, SETDB1, SHANK2, SHC2, SIL1, SIN3B, SLC12A3, SLC22A15, SLC24A2, SLC38A10, SLC44A5, SLC6A1, SLC8A1-AS1, SNORD115-1, SNORD115-2, SNTB2, SNTG2, SNX29, SORCS2, SOX5, SPATA5, SPIDR, SPIRE1, SPTB, SPTBN2, SPTLC3, SRD5A1, SRRM4, ST20, ST20-MTHFS, ST6GAL1, STARD9, STIM1, STK31, STK38, STON1-GTF2A1L, STXBP5-AS1, SUPT3H, SYN3, TAF1L, TAS2R19, TENM2, TENM3, THRB, THSD7B, TIMM23B, TJP2, TLK1, TMCC1, TMED1, TMEM132D, TMEM218, TMEM66, TMTC2, TNRC6B, TPST1, TPTE, TRAPPC9, TRIO, TRPC4AP, TRPM2, TRRAP, TSNARE1, TSPAN15, TSPEAR, TSSC1, TTC28, TTC40, TULP4, TYRO3P, TYSND1, TYW1B, UGGT2, UHRF1, ULK4, UNC5D, UNC79, UNC93A, USP13, USP15, USP34, USP50, VGLL4, VPRBP, VPS53, WDPCP, WDR1, WDR19, WDR36, WDR60, WWOX, XAF1, ZBTB20, ZCWPW2, ZFPM2, ZFYVE9, ZKSCAN5, ZMAT1, ZMYM4, ZNF135, ZNF14, ZNF317, ZNF32, ZNF32-AS1, ZNF32-AS2, ZNF32-AS3, ZNF335, ZNF341, ZNF350, ZNF382, ZNF415, ZNF556, ZNF595, ZNF664-FAM101A, ZNF670, ZNF670-ZNF695, ZNF7, ZNF717, ZNF718, ZNF767P, ZNF808, ZNF845, ZNRF1, ZSWIM5
(I dropped two genes as they are only date-formatted numbers in the supplied Excel sheet).
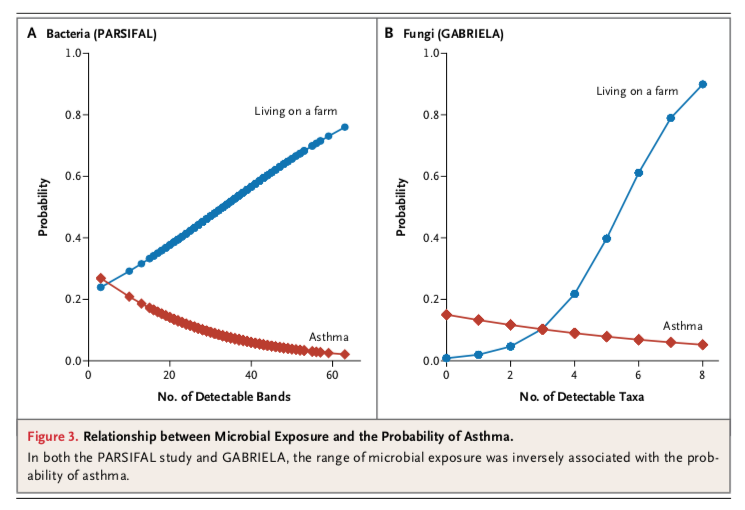
The interesting question for me is if there is an interaction with genes identified earlier in asthma and allergy research. According to the GWAS catalog there are 190 associated genes that match only 9 on the list above: AS1, CLEC16A, CTNNA3, EDIL3, PDE4D, PGAM1P5, SDK1, WDR36. Nothing exciting, in particular no HLA association. WDR36 is the only gene, we published some years ago. I find also only one match (COL15A1) of the 73 low methylation IgE loci published earlier.
Possibly, any of these persistent methylated genes can even stand on its own feet with just one silenced / activated gene being responsible for the pathology in a pedigree. I cannot identify so many signals in the list above, maybe some IL1 related stuff (IL1RAPL2, IL31RA, IRAK1BP1). CD46 at least is a good candidate as it is known that enhanced CD46-induced regulatory T cells will suppress allergic inflammation after allergen specific immunotherapy.
Unexpectedly, there are also no vitamin D related genes, no VDR, no cytochrome P450 enzymes. Nevertheless I recognize a whole bunch of calcium related genes: STIM1 (transmembrane protein that mediates Ca2+ influx), ATP11A + ATP2C1 (ATP dependent Ca2+ transporter), TRPM2 ( another Ca2+ channel), TRPC4AP + RYR1 (sarcoplasmic reticulum calcium channels) and NCALD (a cytosolic calcium transporter).
So would be definitely interesting to test the methylation status of these genes along with vitamin D levels in allergic parents and their kids.