Clemens von Pirquet, when working on horse serum injections, coined the word allergy in 1906. It is largely unknown that his Vienna clinic was also hightly active in “vitamin D” research as described in a new review by Bouillon which cites the Dame Chick lecture Continue reading Pirquet: Allergy and Vitamin D
Category Archives: Vitamins
Is the Loomis Hypothesis wrong?
I remember an old vitamin D book – I believe it was Feldman’s Vitamin D – that argues that if we are going down the Transsahara Route (Algier-Lagos) human skin color gets always darker towards Tamanrasset due to increased solar power- also known known as the Loomis hypothesis (Science 1967).
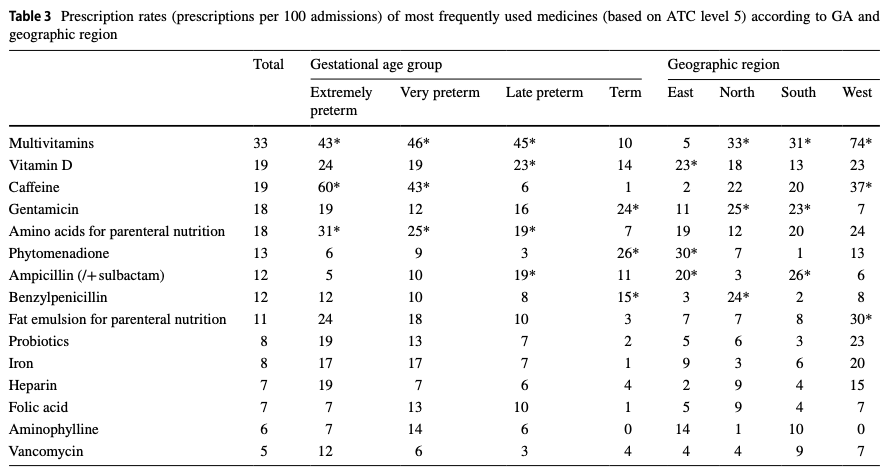
So , let’s have a look at three maps. Solar power first.
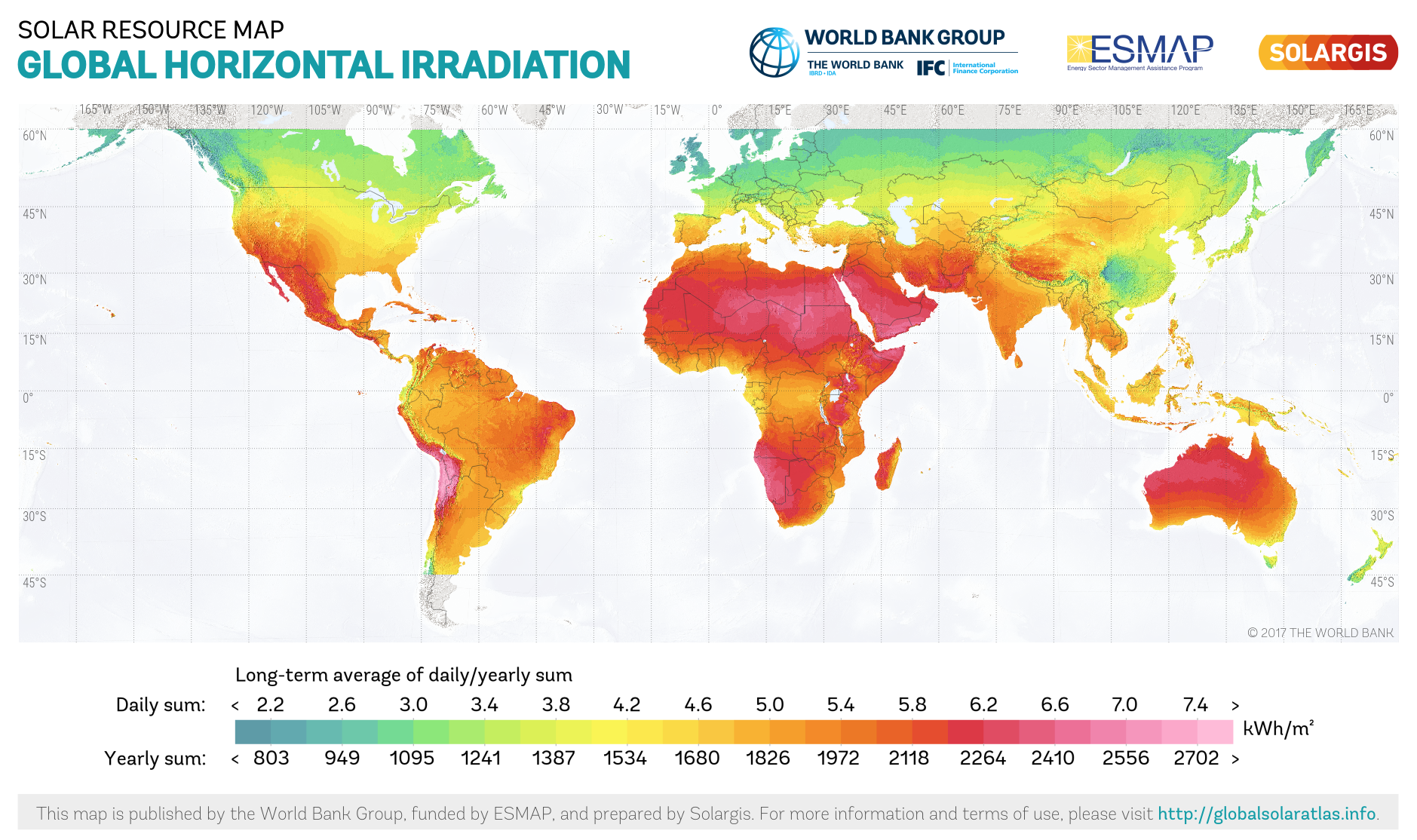
Second, skin tones – the Tamanrasset observation is correct but the overall picture does not match the Loomis hypothesis.
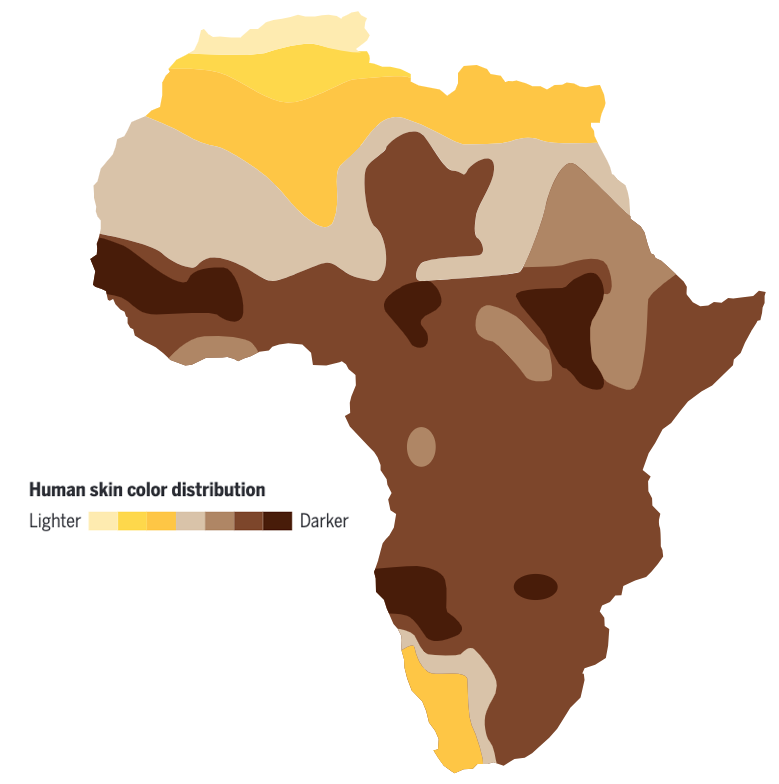
Neither does the new vitamin D map published last week in the Lancet.
Maps are still patchy but let me already believe that the Loomis hypothesis is wrong.
Vitamin D3 in breast milk
Here is the math: 1 µg/L D3 => 40 IU/L D3 => 2,5 nmol/L D3
The detection limit in breast milk is 0,2 nmol/L = 0,08/µg/L = 3,2 IU/L according to vid Streym who measured a median of 0.34 nmol/L 25-OH-D3 in hind milk which is approx 5,4 IU/L.
Li-Chieh Wang gives no detection limit but measures approx 5 ng/mL = 5.000 ng/L = 5 µg/L = 12,5 nmol/L D3 in breast milk equivalent to 200 IU/L, the 40fold amount to vid Streym.
What is correct?
VDR variants are associated with asthma
It is always nice to see an own study 15 years later appearing in a meta-analysis. A new paper in the Annals of Allergy, Asthma and Immunology now shows the results of 17 case–control studies.
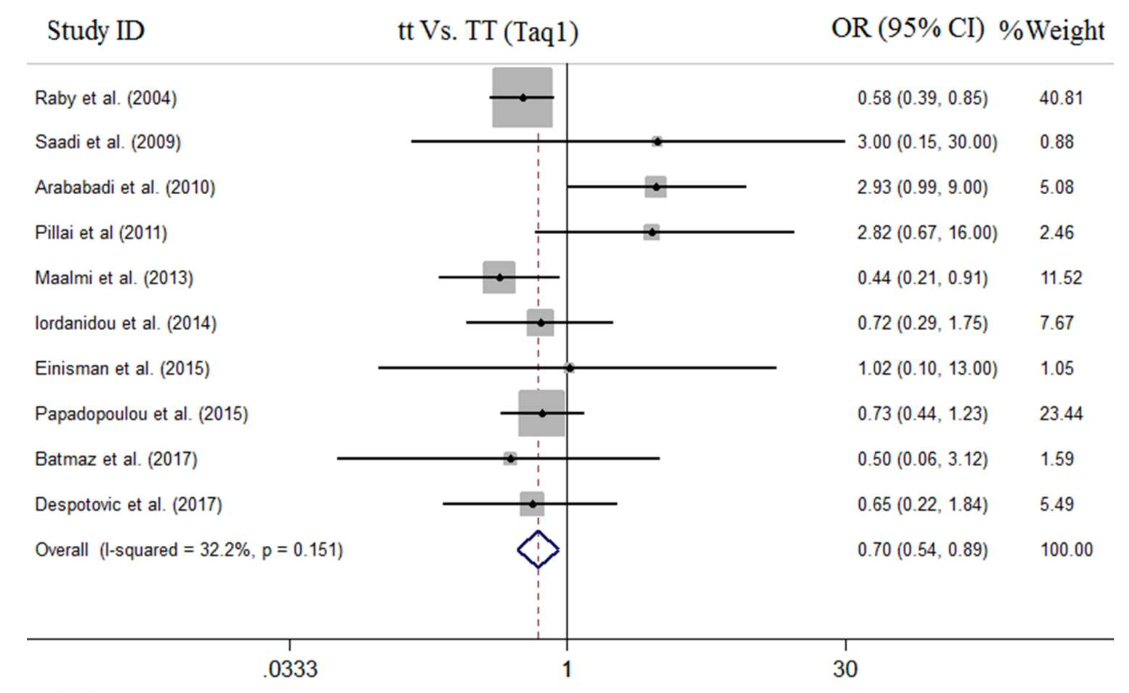
We are in line #1…
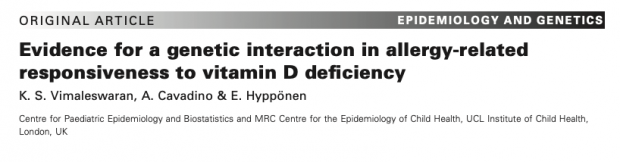
Another nice paper on a genetic interaction is Vimaleswaran et al.
Primary prevention of cow’s milk sensitization and food allergy by avoiding supplementation
A new study by Urashima et al. shows that sensitization to cow’s milk and food allergy, including CMA and anaphylaxis, is preventable by avoiding CMF (cow milk formula) supplementation for at least the first few days of life. Although examined only indirectly in this study, vitamin D supplementation seems to be involved in the sensitization process.
Note to self – here is a list of all vitamin D / allergy related clinical trials following the first case report was Moneret-Vautrin DA, Hatahet R, Kanny G, Ait-Djafer Z. Allergenic peanut oil in milk formulas. The Lancet 1991; 338: 1149. doi: 10.1016/0140-6736(91)92008-p.
1. De Montis G, Gendrel D, Chemillier-Truong M, Dupont C. Sensitisation to peanut and vitamin D oily preparations. The Lancet 1993; 341: 1411. doi: 10.1016/0140-6736(93)90976-N.
2. De Montis G, Gendrel D, Chemillier-Truong M, Dupont C. [Peanut sensitization and oily solution vitamin preparations]. Arch Pediatr 1995;2(1):25-8. doi: 10.1016/0929-693x(96)89804-6.
3. Rueter K, Jones AP, Siafarikas A, Lim EM, Bear N, Noakes PS, et al. Direct infant UV light exposure is associated with eczema and immune development. J Allergy Clin Immunol 2018; in press, doi: 10.1016/j.jaci.2018.08.037.
4. Rosendahl J, Pelkonen AS, Helve O, et al. High-Dose Vitamin D Supplementation Does Not Prevent Allergic Sensitization of Infants. J Pediatr. 2019 Jun;209:139-145.e1. doi: 10.1016/j.jpeds.2019.02.021
The Urashima study is accompanied by a valuable editorial of George du Toit and Kari Nadeau
There is currently a lack of consensus among national allergy societies .. Although the EAACI3 and American Academy of Allergy, Asthma and Immunology (AAAI) currently recommend the use of hypoallergenic formulas in infants at high risk of allergy, the Australian Society of Clinical Immunology and Allergy does not. The EAACI and the AAAI are likely to reconsider their guidelines because results of more re- cent studies have been contradictory. … Guidelines in the United States and United Kingdom recommend routine vitamin D supplementation in all breastfed infants, whereas guidelines in Australia recommend supplementation only in breastfed infants at high risk of vitamin D insufficiency.
Medizin ist keine Wissenschaft sondern eine Kunst
Fragil ist das wissenschaftliche Fundament in der Medizin ja schon immer auch wenn es die hauptsächliche Abgrenzung zur Quacksalberei ist.
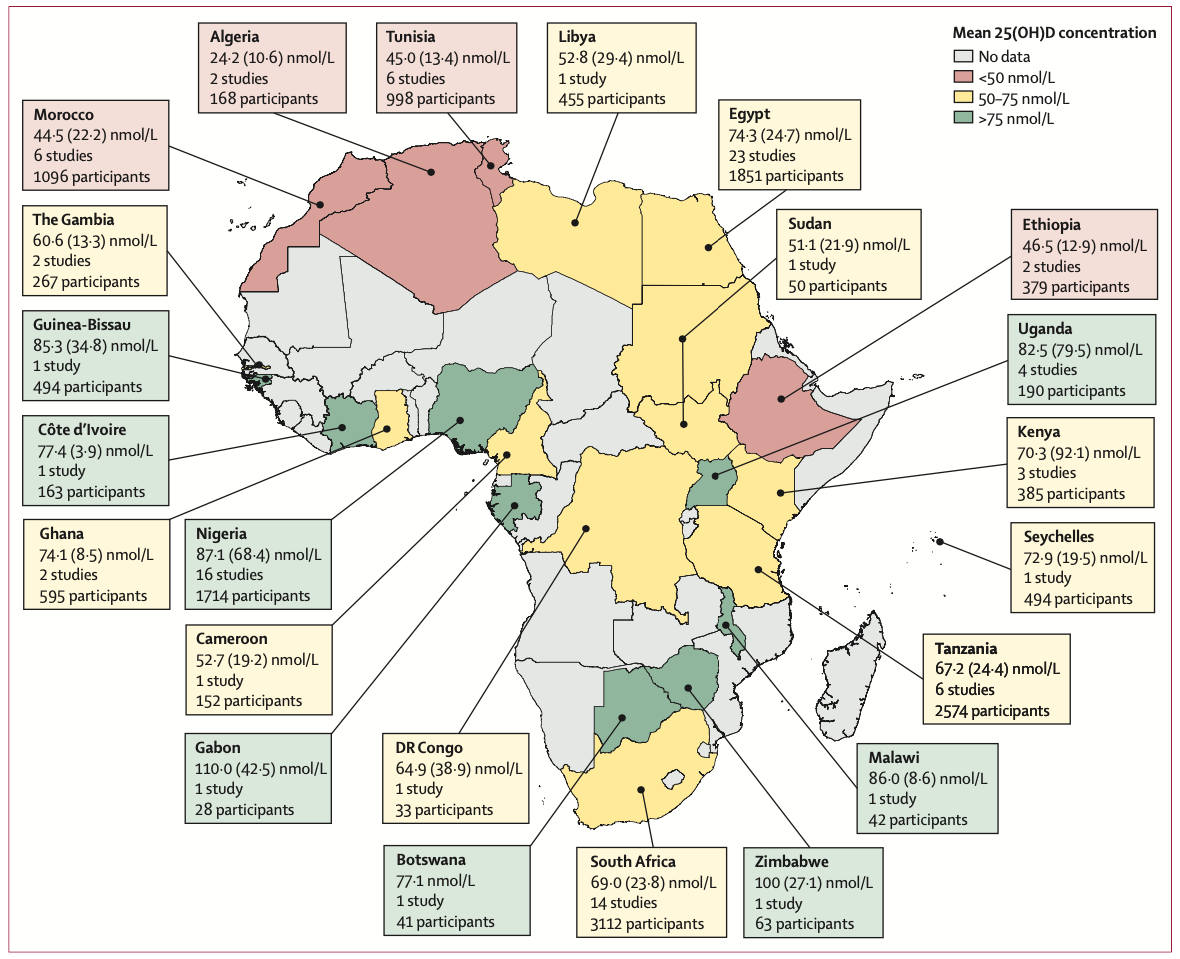
Aber auch wenn man sich manche Fragen der Schulmedizin genauer anschaut, wie zum Beispiel letzte Woche die Empfehlung zu Säuglingsnahrungen oder heute ein Artikel zu Verschreibungen auf Säuglingsstationen, dann ist das weder Wissenschaft noch Kunst sondern bestenfalls industriegeleiteter Aktionismus.
Mesek et al. untersuchten dabei in 21 europäischen Ländern die Verschreibungspraxis auf 89 Stationen. Versorgungsforschung ist ja noch am nähesten an der Realität.
Vitamine sind die am häufigsten verschriebene Pharmaka, wobei unklar ist, warum in machen Regionen 74% und in andern nur 5% Vitamine verschreiben. Wenn es generall notwendig wäre, warum dann nicht 100%? Und wenn es nicht notwendig ist, warum dann nicht 0%?
An open letter to EAACI / PAAM 2019 organizers
Together with many other colleagues I was astonished about the Nestle booth at EAACI / PAAM 2019 conference in Florence.
The advertisement of Nestle for the NAN HA formula (“state-of-the-art routine infant formula“, „proven to reduce the risk of atopic dermatitis“, „long term effects up to 15 years of age“) along with other milk marketing violates recommendations of the WHO and other medical organisations about breast-feeding. None of the claims made is justified from a scientific viewpoint.
Having paid 650 € entry fee for a 3 day conference, it is also not acceptable that Dr Antonella Muraro (Padua) explains in Symposium 9 “Special products for cow’s milk allergy“ that if Nestle would not be sponsoring the event, the congress fees would be even higher.
At present, there is no generally accepted benefit of any baby food on long-term allergy prevention while also the therapeutic benefit is questionable. Commercial baby food may even increase later allergy by including supplements that are itself allergenic.
We therefore recommend a review of the EAACI ethics guidelines of industry sponsorship, and an immediate action against further participation of Nestle at future EAACI allergy congresses.
Allergy protection on farms – why also studies in mice could have failed
There are many immunological differences in humans and mice (follow my link) that are never discussed — not even in Science 2015;349/6252:1106.
Ignoring the long-standing paradox that endotoxin is also acting as a natural adjuvant to atopic inflammation, the credibility of the Science paper is further reduced.
IMHO it is also a strange experimental condition to have all animals on a standard vitamin D diet – a known co-sensitizers – and looking then for A20 which is co-regulated by vitamin D ??
And here is the last argument – more than 90% of studies in mice fail to translate into humans.
Wer lebensgefährlichen Unsinn über Vitamin D verbreitet, wird mit Gefängnis nicht unter 1 Jahr bestraft
“Lebensgefährlicher Vitamin-D-Mangel: Neue Studie veröffentlicht erschreckende Zahlen” wird auf infranken.de/epaper mit passender Werbung für Vitamin D versehen.
Dabei sind wohl mehr Menschen an Überdosierung gestorben , als an einem Vitamin D Mangel (Vitamin D ist im übrigen in hoher Dosierung auch ein Rattengift). Vitamin D Supplemente hatte in vielen Interventionsstudien keinen Vorteil in Bezug auf Mortalität gezeigt, Bluttests dienen nur dem Arzt, der sie durchführt, so die Zusammenfassung im britischen Ärzteblatt BMJ.
Die Mortalität lässt sich nicht durch Vitamin Pillen senken, nur in 2 von 52 Studien gab es eine niedrigere Mortalität und das auch nur in einer Subgruppe (wobei der Effekt in den Originalarbeiten nicht signifikant war).
Und was steckt nun hinter dieser neuen Meldung? Es ist ein Vortragsabstract eines Wiener Facharztes für Haut und Geschlechtskrankheiten, der auf der Tagung einer Diabetesgesellschaft vorgestellt wurde. Also kein Endokrinologe, kein Vitamin Experte, kein Epidemiologe. Damit ist das auch keine Interventionsstudie, nicht mal vernünftig publiziert, nur der Abstract einer “Record Linkage Studie”
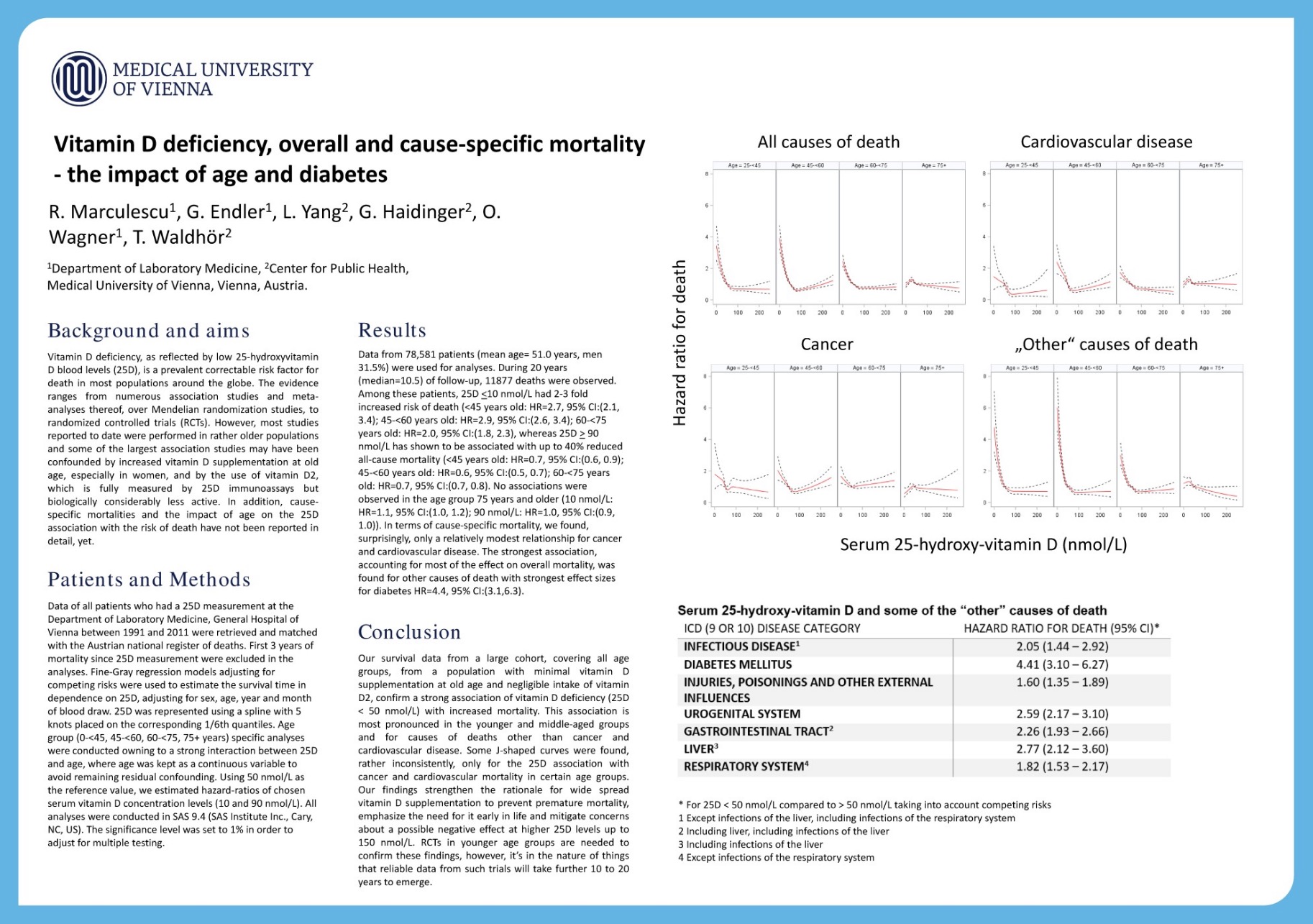
Interessenskonflikte: keine. Sind Vitamin D Assays in Österreich etwa kostenlos?
Dabei wurden Messwerte eines Kliniklabors mit Daten aus dem österreichischen Sterberegister verknüpft. Offensichtlich ist das in Österreich erlaubt, bleibt aber dennoch sinnfrei, wenn man A. weiss, dass Vitamin D ein Aktivitäts- und Inflammationsmarker ist und wenn man B. irgendwann im Leben einmal etwas über Berkson Paradox gehört hat. Warum wohl die ersten 3 Jahre von der Analyse ausgeschlossen wurden, weil die Mortalität da exzessiv gestiegen ist? Ich verstehe die Grafik nicht ganz, da sie nicht zur Methode passt – was ist denn nun die Referenzkategorie für das Hazard Ratio?
Irgendwie hätte es auch den Autoren auffallen müssen – dass es solche exzessiven HRs für Mortalität im echten Leben nicht gibt Natürlich wird jemand früher sterben, der kränker ist, schliesslich ist auch CRP bei Diabetes ein Prädiktor für Mortalität. Aber wen interessiert das ganze denn??
Mittlerweile wird auf Kongressen jeder halbwegs formal korrekte Abstract akzeptiert, um die Kongressgebühren zu kassieren. Auch eurekalert.org sollte das doch wissen, bevor es so eine Information weiter verbreitet. Viele Redaktionen können sich keinen Wissenschaftsredakteur mehr leisten. Und so schlägt dann alles ungefiltert beim Konsumenten ein “Lebensgefährlicher Vitamin-D-Mangel: Neue Studie veröffentlicht erschreckende Zahlen“. Und Herr Marculescu freut sich, da die Vitamin D Tests weiter ansteigen.
17 Okt 2019
infranken.de steigert sich mit derselben Nachricht unter weiteren URLs zur Clickbait Höchstform “Vitamin-D-Mangel kann tödlich sein: Eine Studie veröffentlicht schockierende Zahlen”.
we don’t see things as they are, we see them as we are
There is an interesting meta-analysis at JAMA Pediatrics about vitamin D supplementation during pregnancy and offspring growth, morbidity, and mortality. Nothing special, standardized methodology and even somewhat expected outcome.
In this systematic review and meta-analysis of 24 randomized clinical trials including 5405 individuals, vitamin D supplementation during pregnancy was associated with a lower risk of infants being small for gestational age and improved growth during infancy without an increased risk of fetal or neonatal mortality or congenital abnormality.
More interesting are the vitamin D lobbyists writing the accompanying editorial (Bo Chawes , Klaus Bønnelykke, Hans Bisgaard) . They try by nearly every sentence to devalue the findings of the meta-analysis. They are even getting to the point of
no adverse effects have been found
We don’t see things as they are, we see them as we are.
Es gibt keine Menschenrassen
Es gibt keine Menschenrassen, von Rassen spricht man nur noch im Zusammenhang mit der Tierzucht, wo bestimmte Gruppeneigenschaften gezüchtet werden.
Trotzdem habe ich Probleme mit der Jenaer Erklärung (zitiert nach hpd.de)
Aus genetischer Sicht gebe es im Genom des Menschen “keinen einzigen fixierten Unterschied, der zum Beispiel Afrikaner von Nicht-Afrikanern trennt. Es gibt – um es explizit zu sagen – somit nicht nur kein einziges Gen, welches ‘rassische’ Unterschiede begründet, sondern noch nicht mal ein einziges Basenpaar”. Äußere Merkmale, an denen Rassisten ihre Abwertung von bestimmten Menschengruppen festmachen, seien oberflächliche und biologisch leicht wandelbare Anpassungen an geographische Gegebenheiten. Bis vor 8000 Jahren seien die Menschen in Europa noch “stark pigmentiert” gewesen. Erst durch die Einwanderung von Menschen mit hellerer Hautfarbe aus Anatolien und dem damit einsetzenden Beginn der Landwirtschaft habe sich dies geändert, da es sich bei einer stark pflanzenbasierten Kost im dunklen Winter Europas als evolutionärer Vorteil erwies, hellere Haut zu haben und damit genügend Vitamin D produzieren zu können.
“Die helle Hautfarbe der Menschen im nördlichen Europa ist jünger als 5000 Jahre”, hält die Jenaer Erklärung fest. “Die Verknüpfung von Merkmalen wie der Hautfarbe mit Eigenschaften oder gar angeblich genetisch fixierten Persönlichkeitsmerkmalen und Verhaltensweisen, wie sie in der Blütezeit des anthropologischen Rassismus verwendet wurden, ist inzwischen eindeutig widerlegt. Diese Argumentation heute noch als angeblich wissenschaftlich zu verwenden, ist falsch und niederträchtig. Es gibt auch keinen wissenschaftlich nachgewiesenen Zusammenhang zwischen Intelligenz und geographischer Herkunft, aber einen deutlichen mit sozialer Herkunft.”
Die Erklärung hat natürlich recht, insofern der Rassebegriff nur noch von Rassisten verwendet wird.
Es gibt aber durchaus fixierte phänotypische und genetische Unterschiede in geographischen Regionen – also einzelnen Volksgruppen oder Populationen.
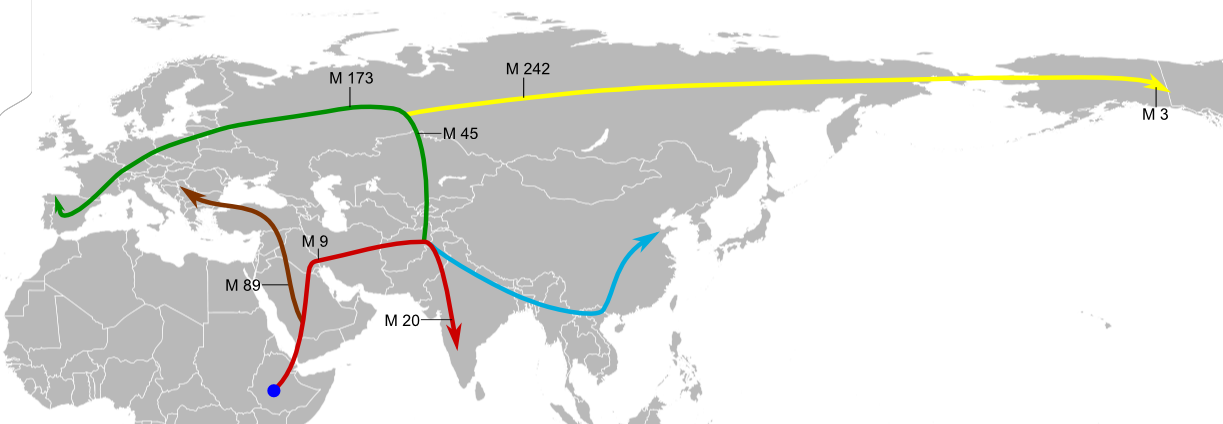
Die Erklärung sagt schliesslich auch, dass Europäer näher verwandt sind mit Ostafrikanern, als Ostafrikaner mit Südafrikanern. Wie sollte eine solche Aussage möglich sein, wenn man keine Marker dafür hätte?
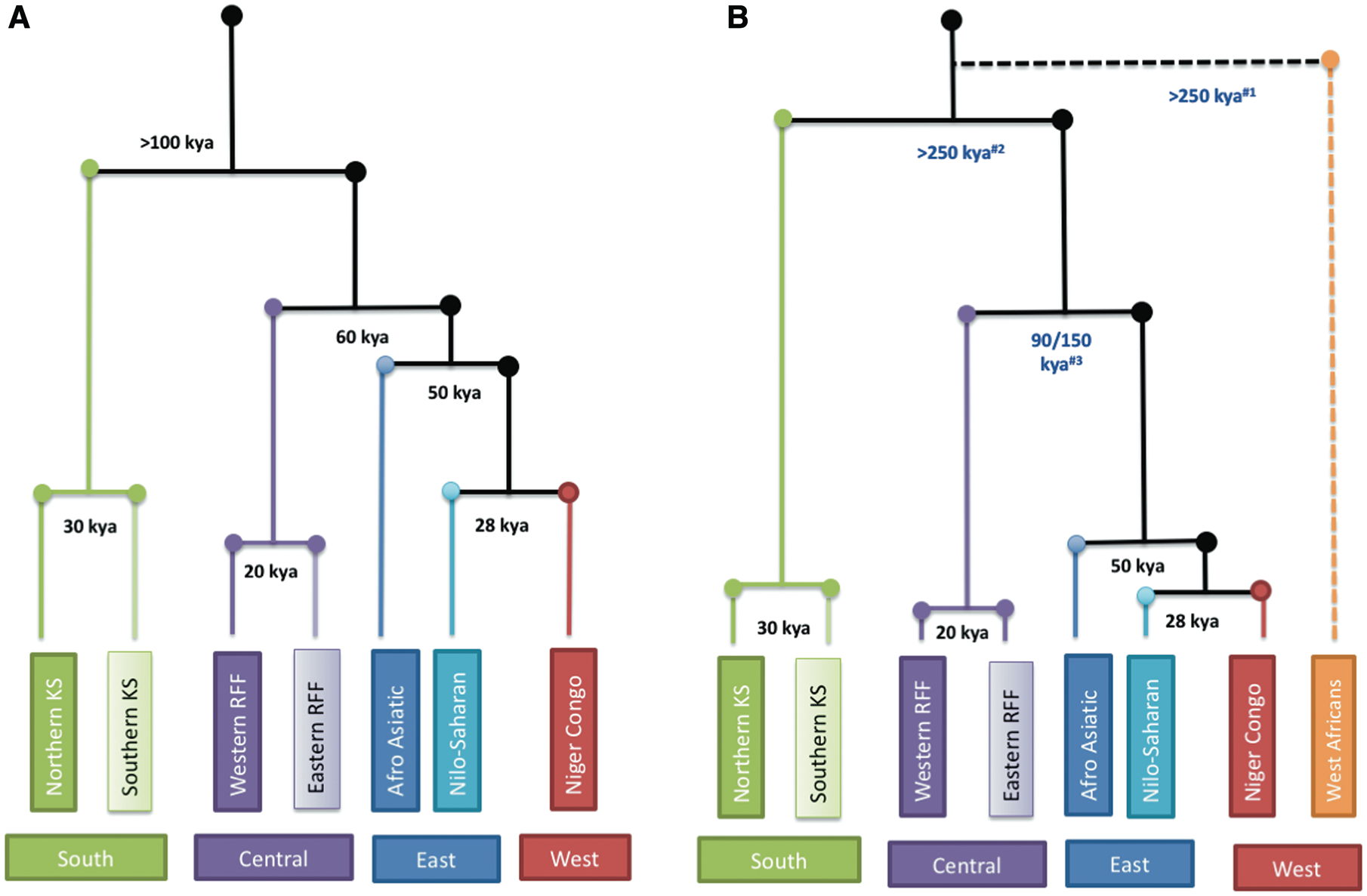
Für Abstammungstheorien wird oft die Kombination von SNP Marker verwandt. Mit Hilfe der “principal component analysis” wurde zum Beispiel der ursprüngliche afrikanische Stammbaum im letzten Jahr revidiert.
“Helle Hautfarbe / bessere Vitamin D Konversion” auch bekannt als Loomis Hypothese als Triebfeder der Evolution ist strittig. Ohne die Literatur zur Pigmentierung der Haut zu rekapitulieren – der Zweck der Pigmentierung ist eher Schutz der Basalzellschicht vor UV Strahlung als eine Limitierung der Vitamin D Produktion. Vitamin D Konversion ist auch ganz ohne starke Pigmentierung selbst limitierend. Sie setzt allenfalls früher, nämlich ca 20 Minuten nach Bestrahlung statt nach 40 Minuten ein.
Nach aktuellem Kenntnisstand stimmt auch nicht, dass dunkle Hautfarbe die ursprüngliche Hautfarbe von H. sapiens in Afrika ist und Europäer mit heller Hautfarbe Mutanten sind (auch wenn es die SZ erneut verbreitet). Helle und dunkle Hautfarbe sind wohl eher die Extreme einer ansonsten mittleren Helligkeit. Der letzte Stand steht dabei in dem Science 2017 Paper von Sarah Tishkoff.
Examining ethnically diverse African genomes, we identify variants in or near SLC24A5, MFSD12, DDB1, TMEM138, OCA2, and HERC2 that are significantly associated with skin pigmentation. … Functional analyses indicate that MFSD12 encodes a lysosomal protein that affects melanogenesis in zebrafish and mice, and that mutations in melanocyte-specific regulatory regions near DDB1/TMEM138 correlate with expression of ultraviolet response genes under selection in Eurasians.
In dieser Liste steht jedenfalls kein einziges Vitamin D – Gen, so dass die Jenaer Erklärung auch hier nicht dem Wissenstand entspricht.
Nachtrag 25.6.2020
Am Sachstand ändert sich nichts wenn die Argumente jetzt wiederholt werden.
Vitamin D polygenic risk score is not associated with any disease
It is one of the minor papers in a minor journal but nevertheless has some big impact: A phenome-wide Mendelian-randomization study of genetically determined vitamin D on multiple health outcomes using the UK Biobank – Int J Epidemiol. 2019 Sep 13
Existing studies suggest that a low vitamin D level is associated with more than 130 outcomes. … We then implemented a Mendelian Randomization-Phenome Wide Association Study (MR-PheWAS) analysis on data from 339 256 individuals of White British origin from UK Biobank. We first ran a PheWAS analysis to test the associations between a 25(OH)D polygenic risk score and 920 disease outcomes…The PheWAS analysis did not identify any health outcome associated with the 25(OH)D polygenic risk score.
The message is clear – we know it for years.
Vitamin D Warnhinweis
Das Deutsche Ärzteblatt hat einen Warnhinweis “Fachgesellschaften warnen vor unkritischem Umgang mit Nahrungsergänzungsmitteln” allem Internet Hype zum Trotz
“Die Werbeaussage, wonach jeder Mensch eine Extraportion Vitamine oder Mineralstoffe zur Aufrechterhaltung der Leistungsfähigkeit und Gesundheit braucht, ist schlicht und einfach falsch“, sagte Jürgen Schölmerich, Facharzt für Gastroenterologie und ehemaliger ärztlicher Direktor und Vorstandsvorsitzender des Universitätsklinikums Frankfurt am Main. Nur für wenige Personengruppen, etwa Schwangere oder Veganer, seien bestimmte Nahrungsergänzungsmittel-Präparate tatsächlich empfohlen.
A waste of 450 papers
https://www.theatlantic.com/science/
In 1996, a group of European researchers found that a certain gene, called SLC6A4, might influence a person’s risk of depression.
It was a blockbuster discovery at the time. The team found that a less active version of the gene was more common among 454 people who had mood disorders than in 570 who did not. In theory, anyone who had this particular gene variant could be at higher risk for depression, and that finding, they said, might help in diagnosing such disorders, assessing suicidal behavior, or even predicting a person’s response to antidepressants.
Back then, tools for sequencing DNA weren’t as cheap or powerful as they are today. When researchers wanted to work out which genes might affect a disease or trait, they made educated guesses, and picked likely “candidate genes.” For depression, SLC6A4 seemed like a great candidate: It’s responsible for getting a chemical called serotonin into brain cells, and serotonin had already been linked to mood and depression. Over two decades, this one gene inspired at least 450 research papers.
But a new study—the biggest and most comprehensive of its kind yet—shows that this seemingly sturdy mountain of research is actually a house of cards, built on nonexistent foundations.
I could give many more examples, from vitamin D associations to the hygiene hype.
Forget about plasma vitamin D measurements
I have written in my recent editorial about the nonsense of plasma vitamin D measurements. A recent case history of a patient with a deleted vitamin D carrier molecule GC now confirms the free-hormone hypothesis. The patient’s plasma 25(OH)D levels was only 0.4% of those in the unaffected sibling.
Despite a lifelong deficiency of vitamin D binding protein, limited sun exposure (for religious reasons), and a diet that was probably lacking sufficient vitamin D, our patient did not have rickets or osteomalacia but rather osteopenia and fragility fractures that occurred in the fifth decade of life.
Another carrier sibling had only two third of the plasma 25(OH)D level compared to the unaffected sibling but showed “no appreciable clinical manifestations”.
So why measure 25(OH)D?